4.03 Structures Of The Male Reproductive System Review Guide
Onlines
Mar 16, 2025 · 7 min read
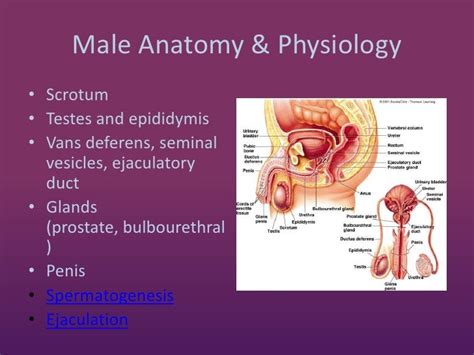
Table of Contents
4.03 Structures of the Male Reproductive System Review Guide
This comprehensive review guide delves into the intricate structures of the male reproductive system. Understanding the anatomy and physiology of each component is crucial for comprehending male reproductive health, fertility, and associated disorders. We'll explore each structure in detail, covering its function, location, and clinical significance.
I. The Testes: The Foundation of Male Fertility
The testes, or testicles, are the primary reproductive organs in males. Their primary function is spermatogenesis, the production of sperm, and steroidogenesis, the production of testosterone.
A. Location and Structure:
The testes are located within the scrotum, a sac-like structure hanging outside the body cavity. This extra-abdominal location is vital because sperm production requires a temperature slightly lower than the core body temperature. Each testis is encased in a tough, fibrous capsule called the tunica albuginea. Internally, the testes are divided into lobules containing seminiferous tubules, where spermatogenesis occurs.
B. Spermatogenesis: The Journey of Sperm Production
Spermatogenesis is a complex, multi-stage process involving the transformation of spermatogonia (stem cells) into mature spermatozoa (sperm). This process is influenced by several hormones, including follicle-stimulating hormone (FSH) and testosterone.
- Spermatogonia: These are diploid cells that undergo mitosis to maintain a pool of stem cells and produce cells that will undergo meiosis.
- Primary Spermatocytes: These are diploid cells that undergo meiosis I, resulting in haploid secondary spermatocytes.
- Secondary Spermatocytes: These undergo meiosis II, resulting in haploid spermatids.
- Spermatids: These undergo spermiogenesis, a process of differentiation that transforms them into mature spermatozoa.
- Spermatozoa: These are the mature sperm cells, consisting of a head (containing the genetic material), a midpiece (containing mitochondria for energy), and a tail (flagellum for motility).
C. Steroidogenesis: The Role of Testosterone
The testes also produce testosterone, a crucial male sex hormone. Testosterone plays a vital role in:
- Development of male secondary sexual characteristics: This includes the growth of facial and body hair, deepening of the voice, and increased muscle mass.
- Spermatogenesis: Testosterone is essential for the process of sperm production.
- Bone growth and density: Testosterone contributes to bone health and strength.
- Libido: Testosterone influences sexual desire.
D. Clinical Significance:
Conditions affecting the testes can lead to infertility, hormonal imbalances, and other health problems. Examples include:
- Cryptorchidism: Failure of one or both testes to descend into the scrotum.
- Testicular cancer: A relatively common cancer in young men.
- Orchitis: Inflammation of the testes.
- Varicocele: Enlargement of the veins within the scrotum.
II. The Epididymis: Maturation and Storage
The epididymis is a long, coiled tube located on the posterior surface of each testis. Its primary functions are:
- Sperm maturation: Sperm that leave the seminiferous tubules are not yet fully functional. The epididymis provides an environment for sperm to complete their maturation process, acquiring motility and fertilizing capacity.
- Sperm storage: The epididymis stores sperm until ejaculation.
A. Structure:
The epididymis is divided into three parts: the head (caput), body (corpus), and tail (cauda). The head receives sperm from the efferent ducts of the testis, while the tail stores mature sperm.
B. Function:
The epididymis's microenvironment plays a crucial role in sperm maturation. It secretes various substances that promote sperm motility, capacitation (the final maturation steps required for fertilization), and survival.
C. Clinical Significance:
Epididymitis, inflammation of the epididymis, is a common condition that can cause pain, swelling, and potentially infertility.
III. The Vas Deferens: The Pathway to Ejaculation
The vas deferens (also called the ductus deferens) is a muscular tube that transports sperm from the epididymis to the ejaculatory duct.
A. Structure and Function:
The vas deferens is a thick-walled tube with strong peristaltic contractions that propel sperm forward. It passes through the inguinal canal, a passageway in the abdominal wall, and enters the pelvic cavity.
B. Clinical Significance:
Vasectomy, a surgical procedure involving cutting and tying the vas deferens, is a highly effective method of male contraception.
IV. The Ejaculatory Ducts and Urethra: The Final Passage
The ejaculatory ducts are formed by the union of the vas deferens and the seminal vesicles. They transport sperm and seminal fluid into the urethra. The urethra serves a dual function, carrying both urine and semen.
A. The Ejaculatory Ducts:
These short ducts pass through the prostate gland and empty into the urethra.
B. The Urethra:
This tube extends from the urinary bladder to the external urethral orifice at the tip of the penis. Its prostatic portion passes through the prostate gland, while its membranous portion passes through the pelvic floor muscles. The spongy (penile) portion runs the length of the penis.
C. Clinical Significance:
Urethral strictures (narrowing of the urethra) can cause difficulty with urination and ejaculation. Prostatitis (inflammation of the prostate gland) can affect the ejaculatory ducts and urethra, leading to pain and discomfort.
V. The Accessory Glands: Contributing to Seminal Fluid
The accessory glands contribute significantly to the volume and composition of seminal fluid, the liquid that carries sperm during ejaculation. These glands include:
A. Seminal Vesicles:
These glands secrete a viscous, alkaline fluid that makes up a significant portion of seminal fluid. This fluid contains fructose (a sugar that provides energy for sperm), prostaglandins (hormone-like substances that may help with sperm transport), and other substances that support sperm survival and motility.
B. Prostate Gland:
The prostate gland, a walnut-sized gland surrounding the urethra, secretes a milky, slightly acidic fluid that contributes to seminal fluid's volume and alkalinity. This fluid contains enzymes that help liquefy the semen after ejaculation, facilitating sperm movement.
C. Bulbourethral Glands (Cowper's Glands):
These small glands located below the prostate secrete a clear, mucus-like fluid that lubricates the urethra prior to ejaculation, neutralizing any residual acidity from urine.
D. Clinical Significance:
Prostatitis (inflammation of the prostate gland), benign prostatic hyperplasia (BPH, non-cancerous enlargement of the prostate), and prostate cancer are significant clinical concerns affecting men. These conditions can cause urinary symptoms, erectile dysfunction, and infertility.
VI. The Penis: The Organ of Copulation
The penis is the male external genitalia responsible for sexual intercourse and urine elimination.
A. Structure:
The penis consists of three cylindrical structures: two corpora cavernosa and one corpus spongiosum. These erectile tissues are filled with blood during sexual arousal, resulting in an erection. The corpus spongiosum contains the urethra and forms the glans penis, the sensitive tip of the penis.
B. Function:
The penis's primary function is to deposit sperm into the female reproductive tract during sexual intercourse. Its erectile tissue allows it to become firm enough for penetration.
C. Clinical Significance:
Erectile dysfunction (ED), the inability to achieve or maintain an erection sufficient for satisfactory sexual intercourse, is a common condition affecting men. Penile cancer, although relatively rare, is a serious condition requiring prompt medical attention. Phimosis (tight foreskin that cannot be retracted) and paraphimosis (retracted foreskin that cannot be returned to its normal position) are conditions requiring medical intervention.
VII. Hormonal Regulation: The Orchestration of Male Reproduction
The male reproductive system is under complex hormonal control. The hypothalamus, anterior pituitary gland, and testes interact in a feedback loop to regulate testosterone production and spermatogenesis.
A. Hypothalamus:
The hypothalamus releases gonadotropin-releasing hormone (GnRH), which stimulates the anterior pituitary gland.
B. Anterior Pituitary Gland:
The anterior pituitary gland releases FSH and luteinizing hormone (LH). FSH stimulates Sertoli cells in the testes to support spermatogenesis, while LH stimulates Leydig cells to produce testosterone.
C. Testes:
Testosterone, produced by Leydig cells, exerts negative feedback on the hypothalamus and anterior pituitary gland, regulating its own production.
D. Clinical Significance:
Hormonal imbalances can disrupt spermatogenesis and testosterone production, leading to infertility and other health problems. Conditions such as Klinefelter syndrome and hypogonadism can affect hormonal levels and male reproductive function.
VIII. Summary and Conclusion
This review guide has provided a comprehensive overview of the structures of the male reproductive system, emphasizing their functions and clinical significance. Understanding the intricate interplay between these structures and their hormonal regulation is crucial for comprehending male reproductive health, fertility, and the various conditions that can affect this system. Further study and consultation with medical professionals are recommended for a more in-depth understanding and for addressing any specific health concerns. Remember that this guide is for informational purposes only and should not be considered medical advice. Always consult a healthcare provider for any health concerns or before making any decisions related to your health or treatment.
Latest Posts
Latest Posts
-
Summary Chronicle Of A Death Foretold
Mar 16, 2025
-
Balzac And The Little Chinese Seamstress Summary
Mar 16, 2025
-
Summary Of Scarlet Letter Chapter 1
Mar 16, 2025
-
Summary Of Chapter 5 Of The Giver
Mar 16, 2025
-
European And American Indian First Encounters Dbq
Mar 16, 2025
Related Post
Thank you for visiting our website which covers about 4.03 Structures Of The Male Reproductive System Review Guide . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
