A Liver Cell Responds To Insulin By
Onlines
Mar 22, 2025 · 6 min read
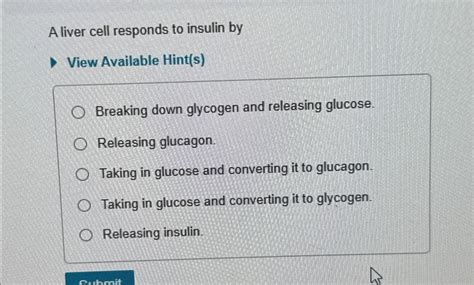
Table of Contents
A Liver Cell Responds to Insulin: A Deep Dive into Hepatic Insulin Signaling
Insulin, a pivotal hormone produced by the beta cells of the pancreas, plays a crucial role in regulating glucose homeostasis. Its effects are widespread, impacting metabolism in various tissues, but its impact on the liver is particularly profound. Understanding how a liver cell responds to insulin is fundamental to comprehending metabolic health and diseases like type 2 diabetes. This article delves deep into the intricate mechanisms by which a hepatocyte (liver cell) senses and responds to insulin, outlining the signaling pathways, downstream effects, and the consequences of dysfunction.
The Insulin Receptor: The Initial Point of Contact
The story begins with the insulin receptor (IR), a transmembrane receptor tyrosine kinase residing on the surface of hepatocytes. This receptor exists as a tetramer, composed of two alpha and two beta subunits. The extracellular alpha subunits bind insulin with high affinity, triggering a conformational change that activates the intracellular beta subunits. This activation is the crucial first step in the cascade of events that follow.
Tyrosine Kinase Activity and Autophosphorylation:
The beta subunits possess intrinsic tyrosine kinase activity. Upon insulin binding, this activity is unleashed, leading to autophosphorylation, a process where the receptor phosphorylates itself on specific tyrosine residues. This autophosphorylation is essential, as it creates docking sites for other signaling molecules, initiating the downstream signaling cascades.
Key Signaling Pathways Activated by Insulin in Liver Cells
Several crucial signaling pathways are activated following insulin receptor autophosphorylation. These pathways orchestrate the diverse metabolic effects of insulin in the liver. The major pathways include:
1. Insulin Receptor Substrate (IRS) Pathway: A Central Hub
The Insulin Receptor Substrates (IRS), particularly IRS-1 and IRS-2, are key adaptor proteins recruited to the phosphorylated insulin receptor. The IR phosphorylates IRS proteins on multiple tyrosine residues, creating binding sites for other signaling molecules like:
-
PI3K (Phosphoinositide 3-Kinase): This enzyme is central to many of insulin's metabolic effects. PI3K is activated upon binding to IRS, leading to the generation of phosphatidylinositol (3,4,5)-trisphosphate (PIP3). PIP3 serves as a docking site for other crucial proteins, including Akt.
-
Grb2 (Growth factor receptor-bound protein 2): Grb2 is involved in activating the Ras/MAPK pathway, influencing gene expression and cell growth. However, its role in hepatic insulin signaling is less prominent compared to the PI3K pathway.
2. The PI3K/Akt Pathway: Orchestrating Glucose Metabolism
The PI3K/Akt pathway is the most extensively studied and arguably the most important pathway downstream of the insulin receptor in the liver. As mentioned, PI3K generates PIP3, which recruits Akt (also known as protein kinase B) to the membrane. Akt is then activated by phosphorylation, triggering a series of downstream events that profoundly impact glucose metabolism:
-
Glycogen Synthase Kinase 3 (GSK3) Inhibition: Akt phosphorylates and inhibits GSK3, an enzyme that normally inactivates glycogen synthase. By inhibiting GSK3, Akt promotes glycogen synthesis, the storage of glucose as glycogen in the liver. This is a crucial step in lowering blood glucose levels.
-
GLUT2 Translocation: Akt indirectly influences the translocation of GLUT2 (Glucose Transporter 2) to the cell membrane. GLUT2 facilitates the uptake of glucose from the portal vein into the hepatocytes. Increased glucose uptake is vital for subsequent glycogen synthesis and other metabolic processes.
-
Forkhead Box Protein O1 (FOXO1) Inhibition: Akt phosphorylates and inhibits FOXO1, a transcription factor that promotes gluconeogenesis (the production of glucose from non-carbohydrate sources). By inhibiting FOXO1, insulin suppresses gluconeogenesis, preventing the liver from unnecessarily releasing glucose into the bloodstream.
3. Other Signaling Pathways: Complementary Roles
While the PI3K/Akt pathway is dominant, other pathways contribute to the overall response of a liver cell to insulin:
-
mTOR (Mammalian Target of Rapamycin): Activated downstream of PI3K, mTOR plays a crucial role in protein synthesis and cell growth. It influences hepatic protein synthesis and contributes to the overall anabolic effects of insulin.
-
MAPK (Mitogen-Activated Protein Kinase) Pathway: As mentioned, the Ras/MAPK pathway is less prominent than PI3K/Akt in hepatic insulin signaling. It's primarily involved in regulating gene expression and cell growth, playing a more secondary role in glucose metabolism.
Downstream Effects: The Metabolic Consequences
The activation of these signaling pathways leads to several crucial metabolic effects in the liver:
-
Increased Glucose Uptake: Insulin promotes glucose uptake by increasing the expression and translocation of GLUT2 transporters to the cell membrane.
-
Enhanced Glycogen Synthesis: Insulin inhibits GSK3, leading to the activation of glycogen synthase and the subsequent storage of glucose as glycogen.
-
Suppressed Gluconeogenesis: Insulin inhibits FOXO1, reducing the production of glucose from non-carbohydrate sources.
-
Stimulated Lipogenesis: Insulin promotes the synthesis of fatty acids from excess glucose, contributing to energy storage.
-
Inhibition of Lipolysis: Insulin inhibits the breakdown of triglycerides, preventing the release of fatty acids into the bloodstream.
-
Increased Protein Synthesis: Through mTOR activation, insulin stimulates protein synthesis, promoting cell growth and repair.
Consequences of Insulin Resistance in the Liver
Insulin resistance, a condition where the liver cells become less responsive to insulin, is a hallmark of type 2 diabetes and metabolic syndrome. In insulin resistance, the signaling pathways described above are impaired, leading to several detrimental effects:
-
Hyperglycemia: Reduced glucose uptake and increased gluconeogenesis result in elevated blood glucose levels.
-
Hyperlipidemia: Impaired lipogenesis and increased lipolysis contribute to elevated levels of triglycerides and free fatty acids in the blood.
-
Hepatic Steatosis (Fatty Liver): Increased lipogenesis and reduced lipolysis lead to the accumulation of fat in the liver, potentially progressing to non-alcoholic fatty liver disease (NAFLD).
-
Increased Inflammation: Insulin resistance is associated with chronic low-grade inflammation in the liver, contributing to the progression of NAFLD and other liver diseases.
-
Increased risk of type 2 diabetes and cardiovascular disease: These metabolic abnormalities increase the risk of developing type 2 diabetes and other cardiovascular complications.
Therapeutic Implications: Targeting Insulin Signaling
Understanding the molecular mechanisms of hepatic insulin signaling is crucial for developing effective therapies for metabolic disorders. Current and future therapeutic strategies aim to:
-
Improve Insulin Sensitivity: Lifestyle modifications (diet and exercise) can enhance insulin sensitivity, restoring normal signaling pathways.
-
Target Specific Signaling Molecules: Drugs that enhance PI3K/Akt signaling or inhibit GSK3 are being investigated to improve glucose metabolism.
-
Reduce Hepatic Inflammation: Targeting inflammation in the liver could help prevent the progression of NAFLD and other liver diseases.
-
Control Blood Glucose Levels: Medications that improve glucose uptake or suppress gluconeogenesis are widely used in the treatment of type 2 diabetes.
Conclusion: A Complex but Crucial Process
The response of a liver cell to insulin is a remarkably intricate process, involving a cascade of signaling events that precisely regulate glucose metabolism and energy homeostasis. Understanding these mechanisms is crucial for comprehending the pathophysiology of metabolic disorders and developing effective therapeutic strategies. Further research into the complexities of hepatic insulin signaling will undoubtedly lead to advancements in the prevention and treatment of diseases like type 2 diabetes and NAFLD. The detailed understanding of insulin's impact on the liver remains a significant area of ongoing research and a crucial aspect of maintaining overall health and well-being.
Latest Posts
Latest Posts
-
A 2 Week Old Infant Is Being Evaluated For Irritability
Mar 23, 2025
-
In Cultural Anthropology The Term Belief Refers To
Mar 23, 2025
-
4 13 Unit Test Chemical Thermodynamics Part 1
Mar 23, 2025
-
Forensic Files Where The Blood Drops Worksheet Answers
Mar 23, 2025
-
The Hound Of The Baskervilles Characters
Mar 23, 2025
Related Post
Thank you for visiting our website which covers about A Liver Cell Responds To Insulin By . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
