An Audit Is Defined By Ich E6 As
Onlines
Apr 01, 2025 · 7 min read
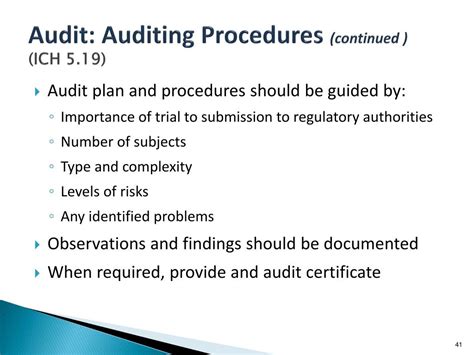
Table of Contents
An Audit Defined by ICH E6: A Deep Dive into Good Clinical Practice
The International Council for Harmonisation of Technical Requirements for Pharmaceuticals for Human Use (ICH) E6 guideline, "Good Clinical Practice (GCP)", is the cornerstone of ethical and scientific quality in clinical trials. A key aspect of GCP, and a critical component of ensuring data integrity and trial reliability, is the audit. This article delves into the ICH E6 definition of an audit, explores its purpose, methodology, and crucial role in maintaining the integrity of clinical research.
What is an Audit According to ICH E6?
ICH E6 doesn't offer a single, concise definition of "audit" in a standalone sentence. Instead, the guideline implicitly defines it through the description of its purpose and process. Essentially, an audit within the context of ICH E6 is a systematic and independent examination of trial-related activities and documents to determine the extent to which the trial is conducted, recorded, and reported in accordance with the protocol, the applicable regulatory requirements, and GCP.
This definition highlights several key aspects:
- Systematic: Audits follow a pre-defined plan and methodology, ensuring a thorough and consistent evaluation. They're not haphazard checks but rather meticulously planned investigations.
- Independent: Auditors must be free from any influence or bias that might compromise their objectivity. This independence ensures an unbiased assessment of the trial's conduct.
- Examination of Activities and Documents: Audits encompass both the actions undertaken during the trial (e.g., subject recruitment, data collection) and the documentation supporting these actions (e.g., case report forms, investigator brochures).
- Compliance with Protocol, Regulations, and GCP: The ultimate goal of an audit is to ascertain whether the trial adheres to the established protocol, relevant regulatory requirements (e.g., those of the FDA, EMA, etc.), and the principles of GCP.
The Purpose of Audits in Clinical Trials
The primary purpose of audits, as implied by the ICH E6 guideline, is to ensure the quality and integrity of clinical trial data. This goal translates into several specific objectives:
- Verification of Compliance: Audits verify that all aspects of the trial, from initial design to final reporting, comply with the protocol, GCP, and applicable regulations. This helps to minimize the risk of flawed data and unreliable results.
- Detection of Deviations: Audits aim to identify any deviations from the protocol, GCP, or regulations. These deviations, even seemingly minor ones, can significantly impact the reliability of the trial's findings.
- Identification of Systemic Issues: By examining a representative sample of trial activities, audits can help identify systemic issues that may affect the quality of the data throughout the trial. This allows for corrective action and prevents recurrence.
- Protection of Human Subjects: Ensuring compliance with GCP protects the rights, safety, and well-being of human subjects participating in the trial. Audits play a critical role in this protection.
- Ensuring Data Reliability: Reliable data is paramount in clinical trials. Audits contribute to data reliability by verifying the accuracy, completeness, and consistency of the collected information.
- Supporting Regulatory Submissions: Audits help support regulatory submissions by providing evidence of compliance with GCP and other requirements. This improves the chances of regulatory approval and minimizes potential delays.
Who Conducts Audits?
Audits can be conducted by various parties, each with a distinct perspective and responsibility:
- Sponsors: Sponsors are typically responsible for conducting or overseeing audits of their investigators. These audits are often referred to as sponsor audits.
- Regulatory Authorities: Regulatory agencies like the FDA or EMA may conduct their own audits to verify compliance with GCP and applicable regulations. These are known as regulatory audits.
- Contract Research Organizations (CROs): CROs, which often manage various aspects of clinical trials, may conduct internal audits to ensure their own processes are compliant. They may also audit their investigators' sites.
- Independent Audit Firms: Independent third-party audit firms specializing in GCP can provide unbiased assessments of trial conduct.
The Audit Process: A Step-by-Step Guide
While the specifics may vary, the general audit process typically involves these steps:
- Planning: This phase involves defining the audit's scope, objectives, and methodology. A detailed audit plan is developed, outlining the specific documents and activities to be reviewed.
- Selection of Sites/Investigators: The audit plan will specify which sites or investigators will be audited. Selection may be based on risk assessment, randomization, or other criteria.
- On-site Visit (if applicable): For many audits, an on-site visit is necessary to review documents, interview personnel, and observe trial activities.
- Document Review: A significant portion of the audit involves a detailed review of relevant documents, including the protocol, case report forms (CRFs), investigator brochures, and other supporting documentation.
- Interviews: Interviews with investigators, study personnel, and other relevant individuals are conducted to clarify information and gain further insight into trial processes.
- Observation: Observation of trial activities, such as subject recruitment or data entry, may also be part of the audit process.
- Reporting: The findings of the audit are documented in a comprehensive audit report, which includes a summary of the audit process, any identified deviations from GCP, and recommendations for corrective action.
- Follow-up: After the report is issued, a follow-up is usually conducted to verify that corrective actions have been implemented.
Types of Audits
Different types of audits exist, each serving a specific purpose:
- Pre-study Audits: These audits assess the preparedness of the site and the investigators before the trial begins. This ensures that the necessary infrastructure and procedures are in place.
- Interim Audits: Conducted during the ongoing trial, interim audits monitor compliance and identify potential issues early.
- Final Audits: These audits are performed at the end of the trial, reviewing all activities and documentation related to the trial's completion.
- Focused Audits: These audits concentrate on a specific aspect of the trial, such as data management or safety reporting.
- Compliance Audits: These audits primarily focus on confirming adherence to regulations, guidelines, and standard operating procedures.
- Quality Audits: These audits have a broader scope, evaluating the overall quality management system and processes of the clinical trial.
Common Audit Findings and Deviations
While the specifics vary widely, some common audit findings and deviations include:
- Incomplete or Missing Documentation: Lack of complete and accurate documentation is a frequent finding.
- Protocol Deviations: Instances where the trial procedures deviated from the protocol.
- Data Integrity Issues: Problems with data accuracy, completeness, and consistency.
- Inadequate Subject Consent: Issues related to informed consent processes.
- Improper Handling of Adverse Events: Inadequate reporting or management of adverse events.
- Insufficient Training of Personnel: Lack of proper training for personnel involved in the trial.
- Failure to Follow Standard Operating Procedures: Deviation from established SOPs.
- Inaccurate Data Entry: Errors or inconsistencies in data entry.
Corrective and Preventive Actions (CAPA)
When deviations are identified during an audit, corrective and preventive actions (CAPA) must be implemented to address the issues and prevent their recurrence. This typically involves:
- Investigating the root cause of the deviation: Identifying the underlying reasons for the non-compliance.
- Developing and implementing corrective actions: Taking steps to correct the immediate issue.
- Developing and implementing preventive actions: Taking measures to prevent the issue from happening again.
- Documenting the CAPA process: Maintaining thorough records of the entire CAPA process.
- Verification of effectiveness: Confirming that the corrective and preventive actions were effective in resolving the issue.
The Importance of Documentation in Audits
Meticulous documentation is paramount throughout the entire clinical trial lifecycle, and it's especially crucial for audits. Without proper documentation, it becomes extremely difficult to demonstrate compliance with GCP and applicable regulations. Key documents include:
- Protocol: The detailed plan for the trial.
- Case Report Forms (CRFs): Forms used to record subject data.
- Informed Consent Forms: Documents obtained from subjects giving their consent to participate.
- Investigator's Brochure: A document describing the investigational product.
- Standard Operating Procedures (SOPs): Documents outlining standard processes and procedures.
- Audit Trails: Records of all actions performed on electronic systems.
Conclusion: Audits as Cornerstones of Good Clinical Practice
Audits, as implicitly defined within the framework of ICH E6 GCP, are indispensable elements in maintaining the integrity and reliability of clinical trials. They provide a systematic and independent assessment of compliance, ensuring the protection of human subjects and the production of trustworthy data. By diligently addressing audit findings and implementing effective CAPA plans, sponsors and investigators can strengthen their commitment to GCP, enhancing the quality of clinical research and contributing to the advancement of medical knowledge. A proactive approach to compliance, with a robust audit program, safeguards not only the trial's success but also the credibility of the entire pharmaceutical industry.
Latest Posts
Latest Posts
-
Which Technology Is Shown In The Diagram
Apr 02, 2025
-
Selecciona La Palabra Que No Esta Relacionada
Apr 02, 2025
-
Refer To The Graphic What Type Of Cabling Is Shown
Apr 02, 2025
-
Activity A Continued From Previous Page
Apr 02, 2025
-
Separate But Equal Movie Questions Answer Key
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about An Audit Is Defined By Ich E6 As . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
