Assignment 5.2 Skeletal System Case Studies
Onlines
Mar 20, 2025 · 8 min read
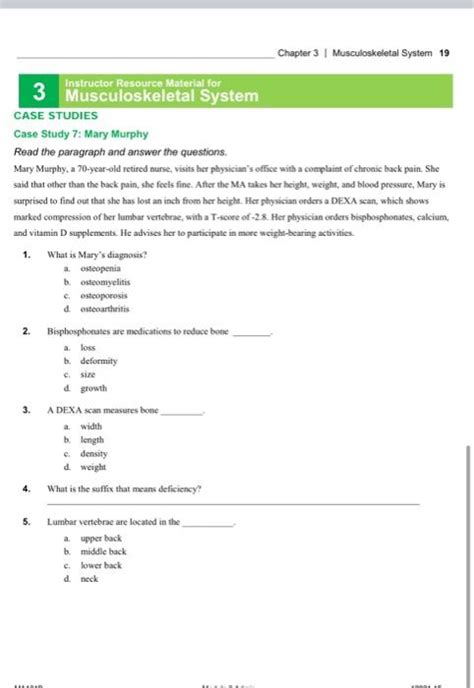
Table of Contents
Assignment 5.2: Skeletal System Case Studies – A Deep Dive
This comprehensive guide delves into the intricacies of Assignment 5.2, focusing on skeletal system case studies. We'll explore various scenarios, analyzing symptoms, identifying potential diagnoses, and outlining appropriate treatment strategies. This guide aims to provide a robust understanding of skeletal system pathologies, diagnostic procedures, and therapeutic approaches. Remember to always consult your textbook and lecture notes for specific details relevant to your course.
Case Study 1: The Young Athlete with Persistent Knee Pain
Patient: A 16-year-old competitive soccer player presents with persistent pain in their right knee, specifically around the patella. The pain began gradually, worsening after intense training sessions. The patient reports feelings of instability and occasional "giving way" of the knee.
Symptoms:
- Localized pain: Primarily around the patella, exacerbated by activity.
- Swelling: Mild to moderate swelling noted in the knee joint.
- Instability: Feeling of the knee "giving way" during activity.
- Crepitus: A crackling or grinding sensation felt or heard during knee movement.
Possible Diagnoses:
- Patellofemoral Pain Syndrome (Runner's Knee): This is a common condition characterized by pain around the kneecap, often associated with overuse, muscle imbalances (particularly weakness in the quadriceps and vastus medialis obliquus), and improper tracking of the patella.
- Osgood-Schlatter Disease: An inflammation of the tibial tubercle (a bony prominence below the kneecap) common in adolescents during growth spurts, particularly in active individuals. It often presents with pain and swelling below the kneecap.
- Meniscus Tear: Though less likely given the gradual onset and location of pain, a meniscus tear could be a possibility, especially if the patient reports a specific twisting injury. A meniscus tear often presents with sharper, more localized pain and often involves locking or catching of the knee.
Diagnostic Procedures:
- Physical Examination: This will assess range of motion, palpation for tenderness, and evaluation of muscle strength and flexibility.
- Imaging: X-rays may rule out fractures or other bony abnormalities. An MRI scan may be necessary to visualize soft tissues such as the menisci and ligaments, providing a clearer picture of potential internal damage.
Treatment Strategies:
- Conservative Management (most likely for Patellofemoral Pain Syndrome or Osgood-Schlatter): This will involve rest, ice, compression, and elevation (RICE protocol), physical therapy to strengthen the quadriceps and improve patellar tracking, and possibly NSAIDs for pain relief. Orthotics may also be considered to improve biomechanics.
- Surgical Intervention (less likely, potentially for a significant meniscus tear): Surgery may be considered if conservative treatment fails, or in the case of a significant meniscus tear or other significant structural damage.
Case Study 2: The Elderly Woman with a Hip Fracture
Patient: A 78-year-old woman falls at home and sustains a fracture of her right hip. She presents with severe pain, inability to bear weight on the affected leg, and significant shortening and external rotation of the leg.
Symptoms:
- Severe pain: Intense pain in the hip and groin area.
- Inability to bear weight: Unable to stand or walk on the affected leg.
- Shortening and external rotation: The affected leg appears shorter and rotated outwards compared to the unaffected leg.
- Deformity: Visible deformity may be present at the hip joint.
Possible Diagnoses:
- Femoral Neck Fracture: This is a common type of hip fracture, occurring in the neck of the femur (thigh bone).
- Intertrochanteric Fracture: This fracture occurs between the greater and lesser trochanters of the femur.
- Subtrochanteric Fracture: This fracture occurs below the lesser trochanter.
Diagnostic Procedures:
- Physical Examination: The characteristic shortening and external rotation of the leg, along with the patient's inability to bear weight, strongly suggest a hip fracture.
- Imaging: X-rays are crucial for confirming the diagnosis and determining the type and location of the fracture.
Treatment Strategies:
- Surgical Intervention (almost always necessary): Surgical repair is typically required to stabilize the fracture and allow for healing. This may involve open reduction and internal fixation (ORIF) using plates and screws, or arthroplasty (hip replacement) depending on the severity of the fracture and the patient's overall health. The goal of surgery is to restore joint congruity, stability, and function.
- Post-Operative Care: This involves pain management, physical therapy to regain mobility and strength, and rehabilitation to improve function and prevent complications.
Case Study 3: The Middle-Aged Man with Back Pain
Patient: A 45-year-old man presents with chronic low back pain that has worsened over the past few months. He reports pain radiating down his right leg, numbness in his foot, and difficulty walking.
Symptoms:
- Chronic low back pain: Pain that has persisted for several months.
- Sciatica: Pain radiating down the leg, often accompanied by numbness and tingling.
- Neurological symptoms: Numbness, tingling, weakness, or decreased reflexes in the affected leg.
- Limited range of motion: Difficulty bending, twisting, or extending the spine.
Possible Diagnoses:
- Lumbar Disc Herniation: A herniated disc in the lumbar spine can compress nerve roots, causing pain, numbness, and weakness in the leg. This is a common cause of sciatica.
- Spinal Stenosis: Narrowing of the spinal canal can compress the spinal cord and nerve roots, leading to pain and neurological symptoms.
- Spondylolisthesis: This is a condition where one vertebra slips forward over another, potentially causing nerve compression and pain.
Diagnostic Procedures:
- Physical Examination: This will assess range of motion, neurological function (reflexes, sensation, strength), and palpation for tenderness.
- Imaging: X-rays can visualize the bony structures of the spine. An MRI scan is often necessary to visualize the discs, spinal cord, and nerve roots, aiding in the diagnosis of disc herniation or spinal stenosis.
Treatment Strategies:
- Conservative Management: This may include rest, ice or heat therapy, over-the-counter pain relievers (NSAIDs), physical therapy (to strengthen core muscles and improve posture), and epidural steroid injections to reduce inflammation.
- Surgical Intervention: Surgery may be considered if conservative treatment fails to provide adequate relief, or if there is significant nerve compression causing neurological deficits. Surgical options may include discectomy (removal of part of the herniated disc), laminectomy (removal of part of the lamina to relieve pressure on the spinal cord), or spinal fusion.
Case Study 4: The Post-Menopausal Woman with Osteoporosis
Patient: A 65-year-old post-menopausal woman presents with a recent history of fractures, including a wrist fracture after a minor fall. She reports increasing back pain and loss of height.
Symptoms:
- Fractures: History of fractures after minimal trauma.
- Back pain: Chronic or intermittent pain in the back.
- Loss of height: Noticeable decrease in height over time.
- Postural changes: Kyphosis (curvature of the spine) may be present.
Possible Diagnoses:
- Osteoporosis: A condition characterized by decreased bone density and increased risk of fractures. This is common in post-menopausal women due to decreased estrogen levels.
Diagnostic Procedures:
- Bone Density Scan (DEXA): This is the gold standard for diagnosing osteoporosis. It measures bone mineral density (BMD) to assess bone strength.
- X-rays: May show compression fractures of the vertebrae.
Treatment Strategies:
- Pharmacological Interventions: This may include bisphosphonates, denosumab, or teriparatide to increase bone density and reduce fracture risk.
- Lifestyle Modifications: This includes weight-bearing exercise, calcium and vitamin D supplementation, and smoking cessation (smoking accelerates bone loss).
- Fall Prevention: Measures to reduce the risk of falls are crucial, including improving home safety and addressing any balance or mobility issues.
Case Study 5: The Child with Developmental Dysplasia of the Hip (DDH)
Patient: A 3-month-old infant is brought to the doctor because of an apparent asymmetry in their hip joints. The parents report that one leg appears shorter than the other.
Symptoms:
- Asymmetry of hip folds: Unequal skin folds in the thighs.
- Limited hip abduction: Difficulty spreading the legs apart.
- Leg-length discrepancy: One leg appears shorter than the other.
- Clicking or popping sensation: A palpable or audible click may be felt or heard when manipulating the hip joint.
Possible Diagnoses:
- Developmental Dysplasia of the Hip (DDH): A condition where the hip joint doesn't develop normally, resulting in instability or dislocation of the hip.
Diagnostic Procedures:
- Physical Examination: The Ortolani and Barlow maneuvers are used to assess hip stability.
- Ultrasound: Ultrasound imaging is useful in infants to assess the hip joint structure and detect DDH. X-rays are less helpful in infants due to the presence of cartilage.
Treatment Strategies:
- Pavlik Harness: This harness is typically used for infants with DDH. It keeps the hips in a flexed and abducted position to allow for proper joint development.
- Closed Reduction: If the harness is ineffective, a closed reduction (manipulation under anesthesia) may be performed to relocate the hip.
- Surgical Intervention: Surgery may be necessary in some cases to correct the hip joint deformity.
Conclusion
These case studies highlight the diverse range of conditions affecting the skeletal system. Accurate diagnosis relies on a thorough patient history, physical examination, and appropriate imaging studies. Treatment strategies vary depending on the specific diagnosis and the severity of the condition, ranging from conservative management to surgical intervention. This comprehensive approach is vital for effective management of musculoskeletal disorders and ensuring optimal patient outcomes. Remember this is for informational purposes only and should not substitute advice from a qualified medical professional. Always consult your healthcare provider for any health concerns.
Latest Posts
Latest Posts
-
You Re Hired To Drive Targeted Traffic
Mar 20, 2025
-
Experience Is The Mother Of Illusion
Mar 20, 2025
-
Unit 6 Energy Resources And Consumption Apes Exam Review
Mar 20, 2025
-
For Each Advancement Cycle Education Service Officers Should Retain
Mar 20, 2025
-
Alien Periodic Table Of Elements Answer Key
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about Assignment 5.2 Skeletal System Case Studies . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
