Ati Comprehensive Physical Assessment Of An Adult
Onlines
Mar 26, 2025 · 7 min read
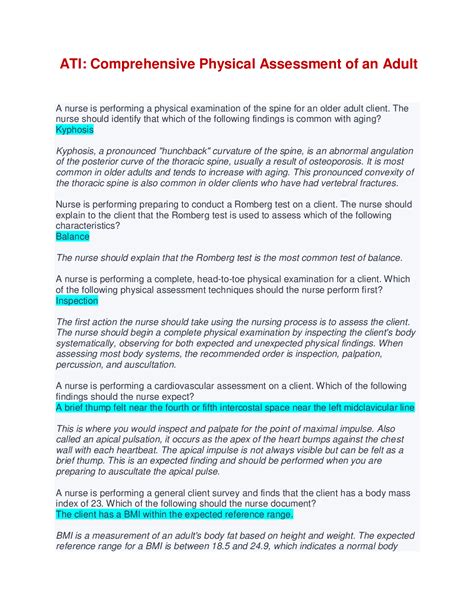
Table of Contents
A Comprehensive Physical Assessment of an Adult: A Guide for Healthcare Professionals
Performing a comprehensive physical assessment is a cornerstone of adult healthcare. It's a systematic process that allows healthcare providers to gather crucial information about a patient's health status, identify potential problems, and develop effective treatment plans. This in-depth guide will walk you through each stage of a comprehensive adult physical assessment, covering essential techniques and considerations. Understanding these steps is vital for accurate diagnosis and quality patient care.
Preparing for the Assessment: Setting the Stage for Success
Before commencing the physical assessment, several preparatory steps are crucial to ensure accuracy, efficiency, and patient comfort:
1. Reviewing the Patient's History:
This initial step is paramount. Carefully review the patient's medical history, including:
- Chief Complaint: Understand the reason for the visit. What are the patient's primary concerns?
- Past Medical History: Note any previous illnesses, surgeries, allergies, and hospitalizations.
- Family History: Identify any hereditary conditions that may be relevant to the current assessment.
- Social History: Consider factors such as lifestyle (diet, exercise, smoking, alcohol consumption), occupation, and social support network. These factors significantly influence health.
- Medication History: Obtain a complete list of current medications, including over-the-counter drugs and supplements. Note dosages and frequency.
2. Establishing Rapport and Consent:
Building a strong rapport with the patient is essential. Explain the purpose and procedure of the assessment clearly and obtain informed consent before proceeding. Respect the patient's privacy and dignity throughout the process. Address any anxieties or concerns the patient might have.
3. Gathering Necessary Equipment:
Ensure you have all the necessary equipment readily available, including:
- Stethoscope: For auscultation of heart, lungs, and bowel sounds.
- Sphygmomanometer: For measuring blood pressure.
- Thermometer: For measuring body temperature.
- Otoscope: For examining the ears.
- Opthalmoscope: For examining the eyes.
- Penlight: For illuminating various body areas.
- Tape measure: For measuring height and circumference.
- Gloves: For maintaining hygiene and preventing infection.
- Examination gown: To provide privacy and ease of access.
- Patient chart/electronic health record: To document findings.
The Comprehensive Assessment: A Step-by-Step Guide
The comprehensive physical assessment typically follows a systematic approach, progressing from general observation to specific examinations of different body systems.
1. General Appearance and Vital Signs:
Begin by observing the patient's overall appearance:
- Level of consciousness: Is the patient alert, oriented, and responsive?
- Apparent state of health: Does the patient appear well or ill? Are there any obvious signs of distress?
- Body habitus: Note the patient's build, posture, and nutritional status.
- Skin: Observe skin color, texture, and any lesions or abnormalities.
- Hygiene: Assess personal hygiene.
Vital Signs: Accurately measure and record the following vital signs:
- Temperature: Oral, rectal, axillary, or tympanic.
- Pulse: Rate, rhythm, and strength.
- Respirations: Rate, rhythm, and depth.
- Blood pressure: Systolic and diastolic readings, in both arms if possible.
- Oxygen saturation (SpO2): Using pulse oximetry.
- Pain Assessment: Using a standardized pain scale (e.g., numerical rating scale, visual analog scale).
2. Neurological Assessment:
Assess the patient's neurological function by evaluating:
- Mental status: Level of consciousness, orientation, memory, attention, and cognitive function.
- Cranial nerves: Assess the function of each cranial nerve (I-XII).
- Motor function: Strength, tone, and coordination of movements in all four extremities. Assess for any tremors or involuntary movements.
- Sensory function: Test light touch, pain, temperature, and vibration sensation in all four extremities.
- Reflexes: Test deep tendon reflexes (biceps, triceps, brachioradialis, patellar, Achilles) and plantar reflexes.
- Balance and gait: Observe the patient's ability to walk and maintain balance.
3. Integumentary Assessment:
Thoroughly examine the skin, hair, and nails:
- Skin: Inspect for color, temperature, moisture, texture, turgor, and lesions (rashes, moles, ulcers, etc.). Assess for any bruising, edema, or signs of infection.
- Hair: Note the distribution, texture, and condition of the hair. Look for any hair loss or unusual patterns.
- Nails: Observe the color, shape, texture, and capillary refill time of the nails. Check for clubbing or any deformities.
4. Head and Neck Assessment:
Examine the head and neck, including:
- Head: Palpate the scalp for tenderness, masses, or lesions.
- Eyes: Assess visual acuity, extraocular movements, pupillary response, and the condition of the conjunctiva and sclera. Use an ophthalmoscope to examine the fundus.
- Ears: Inspect the external ear canal and tympanic membrane using an otoscope. Assess hearing acuity.
- Nose: Examine the nasal passages for patency, discharge, or abnormalities.
- Mouth and throat: Inspect the oral mucosa, teeth, gums, tongue, and pharynx. Note any lesions, inflammation, or abnormalities.
- Neck: Palpate the lymph nodes for enlargement or tenderness. Assess range of motion and palpate the thyroid gland.
5. Cardiovascular Assessment:
Assess the cardiovascular system by:
- Inspecting the precordium: Look for any visible pulsations or abnormalities.
- Palpating the precordium: Feel for apical impulse and any thrills or heaves.
- Auscultating the heart: Listen for heart sounds (S1 and S2), murmurs, rubs, and gallops at various locations on the chest.
- Assessing peripheral pulses: Palpate the radial, brachial, femoral, popliteal, posterior tibial, and dorsalis pedis pulses, noting their rate, rhythm, and strength.
- Assessing blood pressure: Measure blood pressure in both arms.
- Assessing for edema: Check for edema in the extremities.
6. Respiratory Assessment:
Assess the respiratory system by:
- Inspecting the chest: Observe respiratory rate, rhythm, and effort. Note the shape and symmetry of the chest.
- Palpating the chest: Feel for tactile fremitus (vibrations felt during speech).
- Percussing the chest: Percuss the chest to assess lung resonance and identify any areas of consolidation or dullness.
- Auscultating the lungs: Listen to breath sounds in all lung fields, noting any abnormal sounds (wheezes, crackles, rhonchi).
- Assessing for cough: Ask about the presence, character, and severity of any cough.
7. Gastrointestinal Assessment:
Assess the gastrointestinal system by:
- Inspecting the abdomen: Observe the shape, contour, and any visible scars or distension.
- Auscultating the abdomen: Listen for bowel sounds in all four quadrants.
- Percussing the abdomen: Percuss the abdomen to assess tympany and identify any areas of dullness.
- Palpating the abdomen: Gently palpate the abdomen, noting any tenderness, masses, or rigidity.
- Assessing bowel habits: Ask about bowel frequency, consistency, and any changes in bowel habits.
8. Musculoskeletal Assessment:
Assess the musculoskeletal system by:
- Inspecting joints and muscles: Observe for any deformities, swelling, redness, or asymmetry.
- Palpating joints and muscles: Feel for tenderness, warmth, crepitus, or masses.
- Assessing range of motion: Evaluate the range of motion in all major joints.
- Assessing muscle strength: Test muscle strength in all major muscle groups.
- Assessing posture and gait: Observe the patient's posture and gait.
9. Genitourinary Assessment:
Assess the genitourinary system by:
- Inspecting the genitalia: Examine the external genitalia for any abnormalities. (This should be performed sensitively and respectfully, with appropriate draping.)
- Palpating the genitalia: Palpate the inguinal lymph nodes.
- Assessing urinary habits: Ask about urinary frequency, urgency, dysuria, incontinence, and changes in urinary habits.
10. Psychosocial Assessment:
This crucial component addresses the patient's overall well-being and social context:
- Emotional state: Assess mood, affect, and any signs of anxiety or depression.
- Cognitive function: Evaluate mental status and cognitive abilities.
- Social support: Inquire about the patient's social network and support systems.
- Coping mechanisms: Understand how the patient handles stress and challenges.
- Safety concerns: Assess for risk factors for violence, self-harm, or neglect.
Documenting the Assessment: Accuracy and Clarity are Key
Meticulous documentation is vital. Clearly and concisely record all findings, using standardized terminology and objective descriptions. Include:
- Date and time of assessment.
- Patient identification.
- Chief complaint.
- History of present illness.
- Past medical, family, and social history.
- Medication list.
- Vital signs.
- Detailed findings from each body system examination.
- Assessment and plan.
Accurate and comprehensive documentation is not only essential for continuity of care but also protects both the patient and the healthcare provider.
Conclusion: Mastering the Art of the Physical Assessment
The comprehensive physical assessment is a complex yet rewarding process. Mastering this skill requires consistent practice, attention to detail, and a commitment to patient-centered care. By systematically following the steps outlined above, healthcare professionals can effectively gather crucial information, identify potential health problems, and provide the highest quality of patient care. Remember that continuous learning and refinement of your assessment skills are vital for ongoing improvement.
Latest Posts
Latest Posts
-
Table 1 Rate Of Diffusion In Corn Syrup
Mar 29, 2025
-
Comparative Anatomy Of The Domestic Chicken
Mar 29, 2025
-
Stone And Brick Are Substitutes In Home Construction
Mar 29, 2025
-
Damage To The Circled Area May Cause What Symptoms
Mar 29, 2025
-
Ap Bio Unit 7 Progress Check Mcq Part B
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Ati Comprehensive Physical Assessment Of An Adult . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
