Ati Nursing Skill Template Mobility And Immobility
Onlines
Mar 24, 2025 · 8 min read
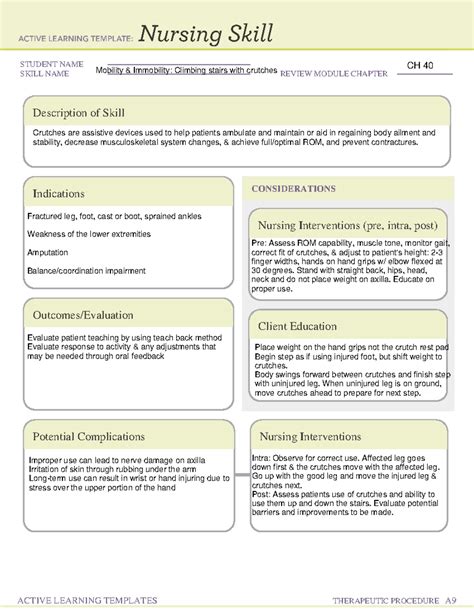
Table of Contents
ATI Nursing Skill Template: Mobility and Immobility – A Comprehensive Guide
Nursing students often find mobility and immobility assessment and intervention challenging. The ATI nursing skill templates provide a structured approach to mastering these crucial skills. This comprehensive guide delves into the ATI template's application to mobility and immobility, covering assessment techniques, nursing interventions, patient education, and potential complications. We’ll explore various mobility issues, from simple gait disturbances to severe immobility requiring extensive care. This guide aims to equip nursing students and professionals with the knowledge and confidence to effectively manage patients facing mobility challenges.
I. Assessment: The Cornerstone of Care
Accurate assessment is the bedrock of effective nursing care for patients with mobility issues. Using the ATI template framework, we'll systematically address key assessment areas.
A. Assessing Mobility
-
Gait: Observe the patient's gait, noting any deviations such as shuffling, unsteady steps, antalgic gait (limping due to pain), wide-based gait, or ataxia (lack of coordination). Document the use of assistive devices like canes, walkers, or wheelchairs. Note the patient's ability to initiate movement, maintain balance, and complete tasks. Consider using a standardized gait assessment tool for greater objectivity.
-
Range of Motion (ROM): Passively and actively assess the patient's ROM in all major joints. Note any limitations, pain, or crepitus (grating sensation). Record the degrees of ROM for each joint using a goniometer if available. Compare findings to the patient's baseline or expected ROM. Document any muscle weakness, contractures, or stiffness.
-
Muscle Strength: Assess muscle strength using a standardized scale, such as the Medical Research Council (MRC) scale. This involves testing the strength of major muscle groups in the upper and lower extremities. Note any asymmetry or significant weakness.
-
Balance: Assess the patient's balance using different tests, such as the Romberg test (standing with eyes closed) or the Timed Up and Go (TUG) test. Observe for any swaying, unsteadiness, or loss of balance. Document the patient's ability to maintain balance in various positions and activities.
-
Activity Tolerance: Determine the patient's activity tolerance by observing their response to physical activity. Note any signs of fatigue, shortness of breath, increased heart rate, or chest pain. Document the duration and intensity of activities the patient can tolerate without undue exertion.
-
Pain: Assess the patient's pain level using a validated pain scale, such as the Numerical Rating Scale (NRS) or the Visual Analog Scale (VAS). Document the location, intensity, quality, and duration of pain. Explore the impact of pain on mobility.
-
Functional Mobility: Evaluate the patient's ability to perform activities of daily living (ADLs), such as bathing, dressing, toileting, eating, and transferring. Use standardized tools like the Katz Index of Independence in Activities of Daily Living or the Barthel Index. Document the level of assistance required for each task.
B. Assessing Immobility
Assessing immobility goes beyond just noting the inability to move. It involves a more holistic approach:
-
Skin Integrity: Meticulously assess the skin for any signs of pressure injuries, including redness, warmth, blanching, or open wounds. Document the location, size, and stage of any pressure injuries using a standardized staging system (e.g., Braden scale). This is crucial for preventing further skin breakdown.
-
Respiratory System: Assess respiratory function, noting respiratory rate, depth, and rhythm. Listen for adventitious breath sounds (e.g., crackles, wheezes). Observe for signs of hypoventilation or atelectasis (collapsed lung). Immobility increases the risk of respiratory complications.
-
Cardiovascular System: Assess heart rate, rhythm, and blood pressure. Observe for signs of orthostatic hypotension (a drop in blood pressure upon standing). Immobility can lead to decreased cardiac output and venous thromboembolism (VTE).
-
Gastrointestinal System: Assess bowel sounds, noting the presence or absence of bowel movements. Inquire about appetite, nausea, or constipation. Immobility can lead to constipation and decreased bowel motility.
-
Musculoskeletal System: Evaluate muscle mass, strength, and tone. Assess for contractures, joint stiffness, and bone density loss (osteoporosis). Prolonged immobility contributes to muscle atrophy, bone loss, and joint contractures.
-
Urinary System: Assess urinary output, noting frequency, urgency, and incontinence. Inquire about urinary tract infections (UTIs). Immobility increases the risk of urinary tract infections and urinary retention.
-
Neurological System: Assess mental status, level of consciousness, and cognitive function. Immobility can lead to depression, anxiety, and cognitive decline.
-
Psychosocial Assessment: Assess the patient's emotional state, coping mechanisms, and social support system. Address issues such as depression, anxiety, isolation, and body image concerns.
II. Nursing Interventions: Promoting Mobility and Preventing Complications
Based on the assessment, appropriate nursing interventions are implemented. This section uses the ATI framework to structure interventions for mobility and immobility.
A. Interventions to Promote Mobility
-
Passive ROM Exercises: If the patient is unable to move independently, perform passive ROM exercises to maintain joint mobility and prevent contractures. Ensure smooth and controlled movements, avoiding any pain.
-
Active ROM Exercises: Encourage the patient to perform active ROM exercises within their capabilities. Start slowly and gradually increase the intensity and duration as tolerated.
-
Ambulation Assistance: Assist the patient with ambulation as needed, using appropriate assistive devices such as walkers, canes, or crutches. Ensure patient safety by using gait belts and providing appropriate support.
-
Transfer Techniques: Use appropriate transfer techniques to help the patient move safely between bed, chair, and toilet. Employ proper body mechanics to avoid injury to both the patient and the caregiver.
-
Progressive Ambulation: Gradually increase the distance and duration of ambulation as the patient's tolerance improves. Monitor for signs of fatigue or distress.
-
Exercise Programs: Develop individualized exercise programs tailored to the patient's abilities and limitations. Consider incorporating aerobic exercises, strength training, and flexibility exercises.
-
Assistive Devices: Provide and educate on the proper use of assistive devices to enhance mobility and independence. This may include canes, walkers, wheelchairs, or adaptive equipment.
-
Adaptive Equipment: Assess the need for adaptive equipment to facilitate ADLs, such as raised toilet seats, grab bars, or long-handled reachers.
B. Interventions to Prevent Complications of Immobility
-
Pressure Relief: Implement pressure relief measures, such as repositioning the patient every 2 hours, using pressure-relieving mattresses or cushions, and providing skin care. Regular skin assessment is paramount to prevent pressure injuries.
-
Deep Breathing Exercises: Teach and encourage deep breathing exercises and coughing techniques to prevent atelectasis and pneumonia. Incentive spirometry can be helpful.
-
Leg Exercises: Encourage leg exercises, such as ankle pumps and foot circles, to improve circulation and prevent deep vein thrombosis (DVT). Consider the use of compression stockings.
-
Hydration and Nutrition: Encourage adequate fluid intake and a balanced diet to maintain hydration and prevent constipation. High-fiber foods are beneficial.
-
Bowel and Bladder Programs: Implement bowel and bladder training programs to help maintain regular bowel and bladder function. This may involve scheduled toileting, fluid management, and medication adjustments.
-
Cognitive Stimulation: Provide cognitive stimulation through activities such as reading, puzzles, and conversation to prevent cognitive decline. Engage the patient in activities they enjoy.
-
Emotional Support: Provide emotional support and address the patient's concerns related to immobility. Refer to social workers or mental health professionals as needed.
-
Pharmacological Interventions: Administer medications as prescribed to manage pain, prevent DVT, treat constipation, and address other medical conditions. Closely monitor for side effects.
-
Fall Prevention: Implement fall prevention strategies, such as removing clutter, ensuring adequate lighting, providing assistive devices, and educating the patient about fall risks.
III. Patient Education: Empowering Patients and Families
Patient and family education is crucial for successful management of mobility and immobility issues.
- Mobility Exercises: Educate patients and families on the importance of regular mobility exercises, demonstrating correct techniques and emphasizing consistency.
- Assistive Devices: Provide thorough instruction on the proper use and care of assistive devices.
- Pressure Injury Prevention: Educate on the risk factors, signs, and prevention of pressure injuries, emphasizing the importance of regular skin checks and pressure relief.
- Nutrition and Hydration: Explain the importance of a balanced diet and adequate fluid intake to promote healing and prevent complications.
- Pain Management: Teach pain management strategies, including medication use, relaxation techniques, and positioning.
- Medication Compliance: Emphasize the importance of medication adherence and the potential side effects of medications.
- Fall Prevention: Educate on fall prevention strategies and risk factors.
- Early Recognition of Complications: Teach patients and families to recognize the signs and symptoms of potential complications, such as respiratory problems, DVT, and pressure injuries, and to seek prompt medical attention.
- Home Safety Modifications: Advise on necessary home modifications to enhance safety and mobility.
IV. Documentation: A Crucial Component of Care
Meticulous documentation is essential to ensure continuity of care and to track the patient's progress. The ATI template guides thorough documentation:
- Assessment Findings: Document all assessment findings objectively and accurately, including gait, ROM, muscle strength, balance, activity tolerance, and functional mobility. Use standardized scales and tools whenever possible.
- Interventions: Document all nursing interventions performed, including ROM exercises, ambulation assistance, pressure relief measures, and patient education. Note the patient's response to interventions.
- Patient Outcomes: Document the patient's progress towards achieving the established goals. Note any improvements in mobility, functional ability, or reduction in complications.
- Communication with the Healthcare Team: Document any communication with other healthcare professionals, including physicians, physical therapists, and occupational therapists.
- Patient Education: Document all patient education provided, including the topics covered and the patient's understanding.
V. Conclusion: Mastering Mobility and Immobility Care
Mastering the assessment and management of mobility and immobility requires a systematic and comprehensive approach. Utilizing the ATI nursing skill template provides a structured framework to guide nursing practice, ensuring consistent and high-quality care. Through thorough assessment, appropriate interventions, effective patient education, and meticulous documentation, nurses can significantly improve the outcomes for patients with mobility challenges and prevent potentially devastating complications. Remember that a holistic approach, considering physical, psychological, and social aspects of care, is vital for optimal patient outcomes.
Latest Posts
Latest Posts
-
Chapter 5 Summary Of Lord Of The Flies
Mar 29, 2025
-
Relias Dysrhythmia Advanced A Test Answers
Mar 29, 2025
-
Which Description Of Synapses Is Not Correct
Mar 29, 2025
-
Which Of The Following Statements Regarding Trench Rescue Is Correct
Mar 29, 2025
-
Fine Print Payday Loan Agreement Answer Key
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Ati Nursing Skill Template Mobility And Immobility . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
