Brian Foster Shadow Health Chest Pain
Onlines
Mar 09, 2025 · 7 min read
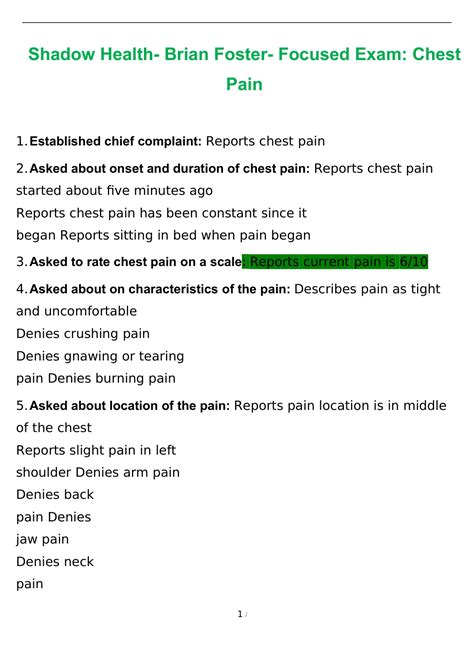
Table of Contents
Brian Foster: A Deep Dive into Shadow Health's Chest Pain Scenario
Shadow Health's virtual patient simulations offer invaluable training for healthcare students. One particularly challenging and realistic scenario is the "Brian Foster" case, focusing on chest pain. This comprehensive guide will dissect the Brian Foster scenario, exploring its nuances, key learning points, and how to approach similar real-world situations. We'll delve deep into the diagnostic process, differential diagnoses, crucial assessment findings, and the importance of effective communication and patient care.
Understanding the Brian Foster Scenario: A Synopsis
Brian Foster, the virtual patient, presents with chest pain, a symptom that demands immediate attention and thorough investigation. The scenario is designed to test your knowledge of cardiac and non-cardiac chest pain causes, emphasizing the critical thinking skills necessary to differentiate between life-threatening conditions and less urgent issues. You'll need to skillfully gather a complete history, perform a focused physical examination, interpret diagnostic test results (often incomplete or ambiguous), and formulate a comprehensive management plan. The complexity of the scenario lies in the ambiguity of the presenting symptoms—a hallmark of real-world clinical practice.
Key Learning Objectives: What You Should Master
Successfully navigating the Brian Foster case will solidify your understanding of several crucial areas:
-
Differential Diagnosis of Chest Pain: The scenario forces you to consider a wide range of potential causes, from acute coronary syndrome (ACS) to less serious conditions like musculoskeletal pain, esophageal spasm, and anxiety. You'll learn to prioritize based on the patient's presentation and risk factors.
-
History Taking and Physical Examination: Effective communication and a meticulous physical exam are pivotal. You need to skillfully elicit relevant information, including the characteristics of the chest pain (location, quality, radiation, associated symptoms, aggravating/relieving factors), past medical history, family history, and current medications. The physical exam should focus on cardiovascular, respiratory, and gastrointestinal systems.
-
Interpreting Diagnostic Tests: The scenario presents various diagnostic test results, some normal and some potentially abnormal. Learning to interpret electrocardiograms (ECGs), cardiac enzyme levels (troponin), and chest X-rays is crucial for accurate diagnosis. Understanding limitations of these tests is equally vital.
-
Clinical Decision-Making: The Brian Foster case challenges your ability to synthesize information, weighing the probabilities of different diagnoses and taking appropriate action based on risk stratification. This includes understanding the urgency of each diagnosis and its potential implications.
-
Communication and Patient Counseling: This is a critical component. You must engage with Brian Foster appropriately, building rapport, explaining procedures, and conveying information in a clear and understandable manner.
Deconstructing the Case: A Step-by-Step Approach
Let's break down how to approach the Brian Foster chest pain scenario effectively:
1. Initial Assessment: The Importance of First Impressions
The initial interaction sets the tone. Begin with open-ended questions to gather information about the chief complaint. Don't interrupt; let Brian Foster describe his chest pain in his own words. Pay close attention to:
- Quality of pain: Is it sharp, dull, aching, crushing, or burning?
- Location of pain: Where exactly is the pain located? Does it radiate to other areas?
- Onset and duration: When did the pain start? How long has it lasted?
- Severity of pain: On a scale of 1 to 10, how would you rate your pain?
- Associated symptoms: Are there any other symptoms like shortness of breath, nausea, vomiting, sweating, dizziness, or lightheadedness?
- Aggravating and relieving factors: What makes the pain worse or better? Rest, movement, certain positions?
2. Detailed History Taking: Uncovering Clues
Beyond the initial assessment, a thorough history is essential. Inquire about:
- Past medical history: Has Brian Foster experienced chest pain before? Does he have any known heart conditions, hypertension, hyperlipidemia, diabetes, or family history of heart disease?
- Medications: What medications is he currently taking? This includes prescription drugs, over-the-counter medications, and herbal supplements.
- Surgical history: Any relevant surgeries, particularly cardiac procedures.
- Social history: Smoking status, alcohol consumption, drug use, occupation, and stress levels. These factors significantly influence risk.
- Allergies: Any known drug allergies?
3. Physical Examination: A Focused Approach
A focused physical examination is crucial to identify potential clues. Pay close attention to:
- Vital signs: Blood pressure, heart rate, respiratory rate, temperature, and oxygen saturation (SpO2).
- Cardiovascular exam: Auscultate for heart sounds (murmurs, rubs, gallops), palpate for apical impulse, and assess for jugular venous distension (JVD).
- Respiratory exam: Auscultate for breath sounds, assessing for crackles, wheezes, or diminished breath sounds.
- Abdominal exam: Assess for tenderness, organomegaly, and bowel sounds. This is important because abdominal issues can mimic chest pain.
- Neurological exam: Assess for any neurological deficits, such as altered mental status or focal weakness.
4. Interpreting Diagnostic Tests: Putting the Pieces Together
The Brian Foster scenario will likely provide you with various diagnostic test results. Critically analyze:
- Electrocardiogram (ECG): Look for ST-segment elevation, ST-segment depression, T-wave inversions, or rhythm disturbances that could indicate myocardial ischemia or infarction.
- Cardiac biomarkers (troponin): Elevated troponin levels are highly suggestive of myocardial damage. The timing of the elevation is crucial.
- Chest X-ray: Assess for signs of pneumonia, pneumothorax, or other pulmonary abnormalities that may cause chest pain.
- Other tests: Depending on the scenario, other tests might be ordered, such as echocardiograms, stress tests, or cardiac catheterization.
5. Differential Diagnosis: Considering the Possibilities
Based on the history, physical exam, and diagnostic test results, create a differential diagnosis, considering the most likely causes of Brian Foster's chest pain:
-
Acute Coronary Syndrome (ACS): This encompasses unstable angina, non-ST-elevation myocardial infarction (NSTEMI), and ST-elevation myocardial infarction (STEMI). This is a life-threatening condition requiring immediate attention.
-
Pericarditis: Inflammation of the pericardium (the sac surrounding the heart) causing sharp, chest pain often worsened by breathing or lying down.
-
Aortic dissection: A tear in the aorta, a life-threatening condition requiring immediate surgical intervention.
-
Pulmonary embolism (PE): A blood clot in the lung, often presenting with shortness of breath and chest pain.
-
Pneumonia: Lung infection causing chest pain and often accompanied by fever, cough, and sputum production.
-
Pneumothorax: Collapsed lung, causing sudden onset of sharp chest pain and shortness of breath.
-
Musculoskeletal pain: Pain from the chest wall muscles, ribs, or cartilage. This is usually non-cardiac in origin.
-
Esophageal spasm: Spasms in the esophageal muscles can cause chest pain similar to angina.
-
Anxiety/Panic attack: Chest pain can be a symptom of anxiety or panic attacks.
6. Management Plan: Prioritizing Patient Care
The management plan depends heavily on the suspected diagnosis. For life-threatening conditions like ACS or aortic dissection, immediate intervention is critical. This may involve:
- Oxygen therapy: To improve oxygenation.
- Analgesia: To manage pain.
- Nitroglycerin: To improve blood flow to the heart (in appropriate situations).
- Antiplatelet agents: To prevent blood clot formation.
- Anticoagulants: To prevent blood clot formation (in appropriate situations).
- Immediate cardiology consultation: For further evaluation and treatment.
For less urgent conditions, the management plan may involve:
- Pain management: Over-the-counter analgesics or prescription medications.
- Lifestyle modifications: Addressing risk factors such as smoking, diet, and exercise.
- Referral to specialists: Depending on the suspected diagnosis (e.g., gastroenterology for esophageal issues).
7. Communication and Patient Education: Building Trust
Throughout the entire process, maintain clear, empathetic communication with Brian Foster. Explain your findings, the proposed diagnosis, and the rationale for the treatment plan in a way he can understand. Answer his questions patiently and address any concerns. Emphasize the importance of follow-up appointments and adherence to prescribed medications.
Beyond the Simulation: Applying Lessons to Real-World Practice
The Brian Foster scenario is a powerful tool for learning, but it is crucial to remember that it’s a simulation. Real-world patients are complex and can present with atypical symptoms. Use this simulation to develop and refine the following skills:
- Critical thinking: Always question your assumptions and be open to alternative diagnoses.
- Clinical reasoning: Synthesize information from various sources to formulate a diagnosis and treatment plan.
- Decision-making under pressure: The urgency of chest pain scenarios demands rapid and accurate decision-making.
- Communication skills: Clear and effective communication is essential for building rapport with patients and their families.
The Brian Foster case in Shadow Health is a valuable tool that equips healthcare students with essential knowledge and skills to approach chest pain scenarios safely and effectively. While the simulation offers a controlled environment to practice, always remember the ethical and clinical responsibility of providing the best possible patient care. Thorough preparation, attention to detail, and a commitment to continuous learning are vital for mastering the art of diagnosis and management in the real world.
Latest Posts
Latest Posts
-
The Company Gave Employees Annual Pay Raises
Mar 10, 2025
-
Symbols For Catcher In The Rye
Mar 10, 2025
-
National Junior Honor Society Recommendation Letter Sample
Mar 10, 2025
-
Pobre Ana English Translation Chapter 3
Mar 10, 2025
-
The Great Gatsby Chapter 3 Fitzgeralds Purpose
Mar 10, 2025
Related Post
Thank you for visiting our website which covers about Brian Foster Shadow Health Chest Pain . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
