Case 2 The Bloated Mrs. Blanc
Onlines
Mar 19, 2025 · 6 min read
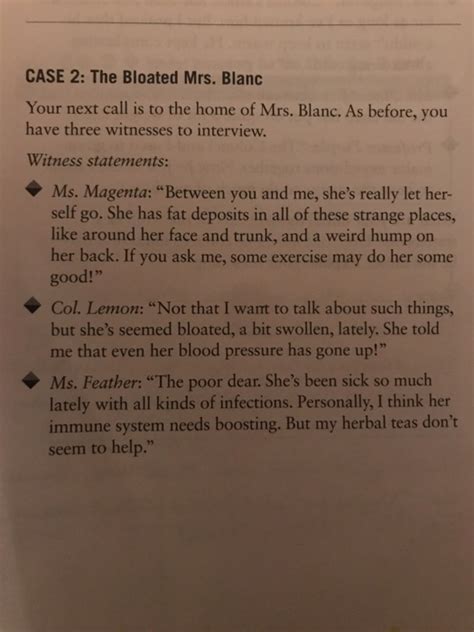
Table of Contents
Case 2: The Bloated Mrs. Blanc – A Deep Dive into a Medical Mystery
This case study delves into the perplexing medical scenario of Mrs. Blanc, a patient presenting with significant abdominal bloating. We will explore the differential diagnoses, investigative procedures, and the crucial reasoning involved in arriving at a definitive diagnosis and treatment plan. Understanding this case will highlight the importance of meticulous history-taking, comprehensive physical examination, and the judicious use of diagnostic tests in managing complex abdominal distension.
Presenting Complaint and Initial Assessment
Mrs. Blanc, a 68-year-old woman, presented to the emergency department complaining of severe abdominal bloating and distension that had progressively worsened over the past three weeks. She described the bloating as constant and uncomfortable, significantly impacting her quality of life. She reported associated symptoms including mild nausea, anorexia (loss of appetite), and increased urinary frequency. She denied any fever, chills, or recent changes in bowel habits (constipation or diarrhea). She had a history of hypertension, well-controlled with medication, but no significant past medical history relevant to her current presentation.
A thorough review of systems revealed no other pertinent findings. On physical examination, Mrs. Blanc appeared mildly distressed due to the abdominal discomfort. Her vital signs were within normal limits. Palpation of the abdomen revealed significant distension with generalized tenderness to palpation, but no rebound tenderness (indicating peritonitis). Bowel sounds were present but slightly diminished. There was no evidence of ascites (fluid buildup in the abdominal cavity).
Differential Diagnoses: A Broad Spectrum of Possibilities
The initial assessment suggested a wide range of potential causes for Mrs. Blanc’s abdominal bloating. The differential diagnosis included:
1. Gastrointestinal Disorders:
- Ovarian Cysts: While less likely given her age, large ovarian cysts can cause significant abdominal distension.
- Ascites (although ruled out on initial exam): Further investigation was needed to definitively exclude this possibility. Causes of ascites include cirrhosis, heart failure, and malignancy.
- Gastroparesis: Delayed gastric emptying can lead to bloating and nausea.
- Irritable Bowel Syndrome (IBS): A common functional gastrointestinal disorder characterized by abdominal pain, bloating, and altered bowel habits. While Mrs. Blanc denied significant changes in bowel habits, it remained in the differential.
- Inflammatory Bowel Disease (IBD): Conditions such as Crohn's disease and ulcerative colitis can cause abdominal distension, but her presentation lacked typical inflammatory symptoms.
- Small Bowel Obstruction: While less likely given the absence of severe pain and vomiting, it could not be entirely ruled out. Obstruction can result from adhesions, hernias, or tumors.
- Large Bowel Obstruction: Similar to small bowel obstruction, but more likely to present with constipation. The absence of constipation made this less probable.
- Pseudocyst (Pancreatic): A fluid-filled cyst in the pancreas can sometimes cause significant abdominal distension, but this is less likely in the absence of other pancreatic symptoms.
2. Gynecological Conditions (less likely given age, but still considered):
- Uterine Fibroids: Benign tumors in the uterus can lead to abdominal bloating and pressure.
- Ovarian Tumors (benign or malignant): While less common in postmenopausal women, ovarian tumors remain a consideration.
3. Other Potential Causes:
- Fluid Retention (generalized edema): This could contribute to abdominal distension but usually presents with edema in other areas as well. No significant edema was noted in Mrs. Blanc’s case.
- Medication Side Effects: Certain medications can cause bloating as a side effect, although a thorough medication review revealed no likely culprits.
- Metabolic Disorders: Rarely, metabolic conditions can cause abdominal distension.
Investigative Procedures: Unraveling the Mystery
To reach a definitive diagnosis, a series of investigations were ordered:
- Complete Blood Count (CBC): To assess for infection, anemia, or other hematological abnormalities. Results were within normal limits.
- Comprehensive Metabolic Panel (CMP): To evaluate liver and kidney function, electrolyte balance, and glucose levels. Results were unremarkable.
- Urinalysis: To rule out urinary tract infection or other urinary abnormalities. The urinalysis was negative.
- Abdominal X-ray: To assess for bowel obstruction, free air (indicating perforation), or other abdominal abnormalities. The x-ray showed significant gas distension in the bowel, but no evidence of obstruction or perforation.
- Abdominal Ultrasound: To visualize abdominal organs and detect potential masses, cysts, or ascites. The ultrasound revealed significant bowel gas distention but no significant masses or ascites. It also revealed a mildly enlarged spleen.
- Computed Tomography (CT) Scan of the Abdomen and Pelvis: A CT scan provides detailed images of abdominal organs and can help identify subtle abnormalities missed on ultrasound. The CT scan revealed significant bowel gas distension and splenomegaly, confirming the ultrasound findings. There were no signs of obstruction, perforation, or masses.
Diagnosis and Treatment: A Complex Puzzle Solved
After a thorough review of the history, physical examination findings, and results of the investigations, a diagnosis of idiopathic chronic intestinal pseudoobstruction was suspected. This condition is characterized by chronic symptoms of bowel obstruction in the absence of a mechanical obstruction. The exact cause remains unclear in many cases, hence the term “idiopathic.” The splenomegaly further suggested a potential systemic component to the disorder.
Treatment of idiopathic chronic intestinal pseudoobstruction is largely supportive and aims to manage symptoms. For Mrs. Blanc, the treatment plan included:
- Dietary Modifications: A low-residue diet was recommended to minimize bowel distension and discomfort.
- Prokinetic Agents: Medications to stimulate bowel motility were prescribed to improve gastric emptying and reduce bloating.
- Antiemetic Medications: Medications to reduce nausea were provided as needed.
- Regular Follow-up: Close monitoring of symptoms and adjustments to the treatment plan as needed.
- Pain Management: Over-the-counter analgesics were recommended for pain relief.
- Referral to Gastroenterology: A referral to a gastroenterologist was made for ongoing management and further investigations to explore the underlying cause of the splenomegaly. This could potentially include investigations such as a colonoscopy to completely rule out any structural issues within the colon itself and more advanced imaging.
Discussion: Uncommon Presentations and Diagnostic Challenges
This case highlights several important points in the diagnosis and management of abdominal distension:
- The importance of a thorough history and physical examination: These are crucial first steps in guiding further investigations.
- The need for a comprehensive differential diagnosis: Abdominal distension can have numerous causes, and clinicians must consider a wide range of possibilities.
- The judicious use of diagnostic tests: While investigations are necessary, it's crucial to avoid unnecessary tests. The sequence of tests should be guided by the clinical suspicion and the findings of previous investigations.
- The challenges in diagnosing idiopathic conditions: In many cases, an underlying cause cannot be identified, making diagnosis and management more challenging.
- The importance of a multidisciplinary approach: Managing complex conditions such as idiopathic chronic intestinal pseudoobstruction often requires collaboration among multiple specialists.
Conclusion: A Case of Persistent Intrigue
Mrs. Blanc’s case presented a diagnostic puzzle that demanded a systematic and thorough approach. The astute clinical reasoning, combined with a stepwise investigation, ultimately led to a likely diagnosis and a tailored treatment plan. This case serves as a valuable reminder of the importance of thoroughness, careful observation, and a collaborative approach in managing complex medical mysteries. While a definitive answer to the underlying etiology of the splenomegaly and the idiopathic chronic intestinal pseudoobstruction remains elusive in this specific case, the comprehensive approach detailed allowed for a significant improvement in Mrs. Blanc's quality of life. Further investigations through referral to a specialist will likely lead to a more nuanced understanding of the underlying issue, potentially leading to more targeted and specific treatment strategies in the future. The focus remains on managing symptoms effectively and ensuring patient well-being.
Latest Posts
Latest Posts
-
A Company Receives 10 000 Indeed
Mar 19, 2025
-
To Kill A Mockingbird Chapter 18 Summary
Mar 19, 2025
-
El Equipo Favorito De Valentina Es El Real Madrid
Mar 19, 2025
-
Documentation For Precertification Can Include Which Of The Following
Mar 19, 2025
-
Differential White Blood Cell Count Data Table Answers
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about Case 2 The Bloated Mrs. Blanc . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
