Chronic Kidney Disease Hesi Case Study
Onlines
Mar 28, 2025 · 6 min read
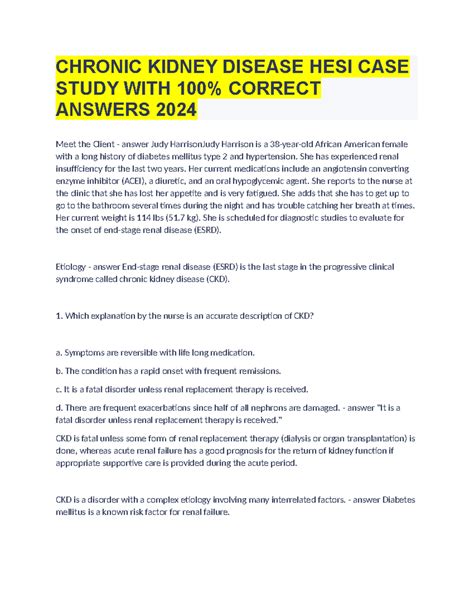
Table of Contents
Chronic Kidney Disease: A Comprehensive HESI Case Study Analysis
Chronic Kidney Disease (CKD) is a progressive and often insidious condition characterized by a gradual decline in kidney function. Understanding CKD requires a multifaceted approach, incorporating knowledge of pathophysiology, clinical manifestations, diagnostic testing, and management strategies. This article delves into a hypothetical HESI case study focusing on a patient with CKD, providing a detailed analysis of the presenting symptoms, diagnostic findings, potential complications, and appropriate nursing interventions. We will explore the intricacies of CKD management, emphasizing the importance of interprofessional collaboration and patient education.
The Case Study: Mrs. Jones's Journey with CKD
Mrs. Jones, a 68-year-old female with a history of type 2 diabetes mellitus and hypertension, presents to the clinic complaining of increasing fatigue, shortness of breath, and lower extremity edema for the past three months. She reports decreased urine output and experiencing nocturia. She admits to non-compliance with her prescribed medications for diabetes and hypertension. Her medical history also reveals a family history of kidney disease.
Initial Assessment and Vital Signs:
Upon assessment, Mrs. Jones appears pale and lethargic. Her vital signs reveal:
- Blood Pressure: 160/90 mmHg
- Heart Rate: 98 bpm
- Respiratory Rate: 22 breaths/min
- Temperature: 98.6°F (37°C)
- Oxygen Saturation: 94% on room air
Physical Examination: reveals crackles in the lung bases, indicating fluid overload. Her lower extremities exhibit significant pitting edema. She also exhibits signs of dehydration.
Diagnostic Evaluation: Unraveling the Mystery of Mrs. Jones's Condition
To accurately diagnose and stage Mrs. Jones’s kidney disease, several diagnostic tests are crucial:
1. Blood Urea Nitrogen (BUN) and Serum Creatinine Levels:
These are essential markers of kidney function. Elevated BUN and creatinine levels indicate impaired glomerular filtration rate (GFR), a hallmark of CKD. High levels suggest that the kidneys are not effectively filtering waste products from the blood.
2. Estimated Glomerular Filtration Rate (eGFR):
The eGFR is a calculation that estimates the GFR, providing a more precise measure of kidney function. It's calculated using serum creatinine levels, age, sex, and race. A decreased eGFR indicates reduced kidney function and is used for CKD staging.
3. Urinalysis:
Urinalysis helps assess the presence of proteinuria (protein in the urine), hematuria (blood in the urine), and other abnormalities that can indicate kidney damage. Proteinuria is a key indicator of kidney damage and is often seen in CKD.
4. Electrolyte Panel:
This panel measures serum levels of electrolytes such as potassium, sodium, calcium, and phosphorus. Electrolyte imbalances are common in CKD due to impaired renal excretion. Hyperkalemia (high potassium) can be particularly dangerous and life-threatening.
5. Complete Blood Count (CBC):
A CBC helps assess the patient's overall hematologic status. Anemia is frequently observed in CKD due to reduced erythropoietin production by the damaged kidneys.
Staging CKD: Understanding the Progression
Based on the eGFR and the presence of albuminuria, CKD is staged from 1 to 5, with stage 5 representing End-Stage Renal Disease (ESRD). Mrs. Jones's condition, based on her symptoms and initial tests, likely falls within stages 3 or 4.
Potential Complications: Navigating the Risks
CKD significantly increases the risk of various complications, including:
1. Cardiovascular Disease (CVD):
CKD patients are at significantly increased risk of CVD due to hypertension, hyperlipidemia, and left ventricular hypertrophy. This risk increases with the severity of CKD.
2. Anemia:
The reduced production of erythropoietin leads to anemia, causing fatigue, weakness, and shortness of breath.
3. Electrolyte Imbalances:
Hyperkalemia, hyperphosphatemia, and hypocalcemia are common in CKD and can lead to cardiac arrhythmias, muscle weakness, and bone disease.
4. Bone Disease:
CKD-mineral bone disorder (CKD-MBD) is a common complication characterized by disturbances in calcium, phosphorus, and parathyroid hormone levels, leading to bone abnormalities.
5. Renal Osteodystrophy:
A specific type of bone disease caused by CKD, resulting in weakened bones and increased risk of fractures.
6. Infections:
Impaired immune function in CKD increases susceptibility to infections.
7. Uremic Symptoms:
As kidney function declines, uremic toxins accumulate in the blood, leading to symptoms such as nausea, vomiting, fatigue, and itching.
Nursing Management: A Multifaceted Approach
Nursing care for Mrs. Jones requires a holistic approach, encompassing assessment, intervention, education, and collaboration.
1. Fluid and Electrolyte Management:
Strict monitoring of fluid intake and output is essential, particularly given Mrs. Jones’s edema. Dietary modifications may be necessary to restrict sodium and potassium intake.
2. Medication Management:
Mrs. Jones needs strict adherence to her prescribed medications for diabetes, hypertension, and any other necessary medications for CKD management. This may include antihypertensive agents, phosphate binders, and erythropoietin stimulating agents.
3. Nutritional Support:
A renal diet, low in protein, phosphorus, potassium, and sodium, is essential. Dietitian consultation is crucial for providing individualized dietary recommendations.
4. Monitoring for Complications:
Close monitoring of vital signs, weight, electrolyte levels, and urine output is necessary to detect and manage potential complications promptly.
5. Patient Education:
Comprehensive patient education is essential, covering disease management, medication regimen, dietary restrictions, potential complications, and the importance of regular follow-up appointments.
6. Psychosocial Support:
CKD can significantly impact a patient's quality of life. Providing psychosocial support, including counseling and support groups, can help Mrs. Jones cope with the emotional and psychological challenges of living with CKD.
7. Collaboration with Interprofessional Team:
Effective management of CKD requires collaboration with a multidisciplinary team, including nephrologists, dietitians, social workers, and other healthcare professionals.
Advanced CKD Management: Considering Dialysis
If Mrs. Jones’s kidney function continues to decline, she may eventually require dialysis. Dialysis is a life-sustaining treatment that removes waste products and excess fluid from the blood when the kidneys can no longer perform these functions effectively. Two main types of dialysis exist:
1. Hemodialysis:
This involves filtering the blood through an artificial kidney machine (dialyzer) outside the body. Hemodialysis is typically performed three times a week in a dialysis center or at home.
2. Peritoneal Dialysis:
This involves using the patient's own peritoneal membrane (lining of the abdominal cavity) as a filter. Dialysis fluid is infused into the abdomen and then drained after several hours. Peritoneal dialysis can be performed at home.
Prognosis and Long-Term Management: Looking Ahead
The prognosis for CKD varies depending on the stage of the disease, the presence of complications, and the effectiveness of treatment. Early diagnosis and aggressive management can slow the progression of CKD and improve the patient's quality of life. Long-term management focuses on managing symptoms, preventing complications, and maintaining as much residual kidney function as possible. Regular monitoring of kidney function, blood pressure, and other vital parameters is essential. Regular follow-up appointments with nephrologists, dietitians, and other healthcare professionals are crucial. Adherence to medication regimens, dietary restrictions, and lifestyle modifications is paramount for slowing disease progression.
Conclusion:
Mrs. Jones's case study highlights the complexity of CKD and the importance of early diagnosis, prompt management, and comprehensive patient care. Successful management of CKD requires a multidisciplinary approach involving close monitoring, medication management, nutritional support, patient education, and collaborative teamwork. Understanding the pathophysiology, clinical manifestations, diagnostic tests, and potential complications of CKD is essential for healthcare professionals providing care for patients with this chronic condition. This case study underscores the crucial role nurses play in providing comprehensive care to patients with CKD, improving their quality of life, and slowing disease progression. It emphasizes the need for patient education and psychosocial support to navigate the challenges of living with this chronic condition.
Latest Posts
Latest Posts
-
Domain 3 Lesson 2 Fill In The Blanks
Mar 31, 2025
-
The Outsiders Book Chapter 4 Summary
Mar 31, 2025
-
2 2 Tangent Lines And The Derivative Homework Answer Key
Mar 31, 2025
-
Agent Roderick Enrolls Retiree Mrs Martinez
Mar 31, 2025
-
Unit 7 Homework 4 Rhombi And Squares Answer Key
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about Chronic Kidney Disease Hesi Case Study . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
