Complete The Missing Parts Of The Table On Diabetes Mellitus
Onlines
Mar 24, 2025 · 8 min read
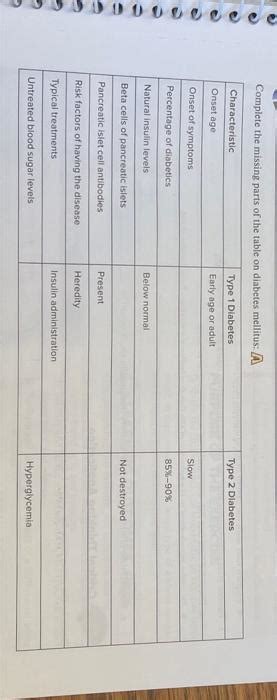
Table of Contents
Completing the Missing Parts of the Table on Diabetes Mellitus: A Comprehensive Guide
Diabetes mellitus, a chronic metabolic disorder characterized by elevated blood glucose levels, affects millions worldwide. Understanding its various types, complications, and management strategies is crucial for effective healthcare. This article aims to comprehensively address the missing parts of a hypothetical table on diabetes mellitus, providing a detailed overview of this complex condition.
I. Types of Diabetes Mellitus
| Type of Diabetes | Description | Characteristics | Risk Factors | Complications | Management |
|---|---|---|---|---|---|
| Type 1 Diabetes | Autoimmune destruction of pancreatic beta cells | Absolute insulin deficiency, hyperglycemia, ketoacidosis prone | Genetics, autoimmune diseases | Cardiovascular disease, nephropathy, neuropathy, retinopathy | Insulin therapy, dietary management, regular monitoring |
| Type 2 Diabetes | Insulin resistance and relative insulin deficiency | Hyperglycemia, gradual onset, often asymptomatic initially | Obesity, family history, physical inactivity, ethnicity | Cardiovascular disease, nephropathy, neuropathy, retinopathy, foot ulcers | Lifestyle modifications (diet, exercise), oral hypoglycemic agents, insulin therapy |
| Gestational Diabetes | Impaired glucose tolerance during pregnancy | Hyperglycemia during pregnancy, resolves after delivery, increased risk of type 2 diabetes later | Pregnancy, obesity, family history | Macrosomia, birth trauma, increased risk of type 2 diabetes in mother and child | Dietary management, insulin therapy if needed |
| Other Specific Types | Rare forms of diabetes due to genetic defects or other conditions | Variable depending on the underlying cause | Genetic mutations, pancreatic diseases | Varies depending on the specific type | Varies depending on the specific type, often requiring specialized treatments |
A. Type 1 Diabetes: Autoimmune Assault on Insulin Production
Type 1 diabetes, formerly known as juvenile diabetes or insulin-dependent diabetes, is an autoimmune disorder. The body's immune system mistakenly attacks and destroys the insulin-producing beta cells in the pancreas. This leads to an absolute deficiency of insulin, the hormone responsible for regulating blood glucose levels. Consequently, glucose cannot enter the body's cells for energy, leading to persistently high blood sugar (hyperglycemia).
Characteristics: The onset of type 1 diabetes is typically abrupt, often presenting with classic symptoms like:
- Polyuria: Frequent urination due to the body attempting to excrete excess glucose.
- Polydipsia: Excessive thirst due to fluid loss from polyuria.
- Polyphagia: Increased hunger despite weight loss due to the inability of cells to utilize glucose for energy.
- Weight loss: Unintentional weight loss despite increased food intake.
- Fatigue: Weakness and tiredness due to cellular starvation.
Risk Factors: While the exact cause remains unknown, genetic predisposition and environmental factors play a role. Individuals with a family history of autoimmune diseases are at increased risk. Viral infections have also been implicated in triggering the autoimmune response.
B. Type 2 Diabetes: A Battle Against Insulin Resistance
Type 2 diabetes, formerly known as adult-onset or non-insulin-dependent diabetes, is far more prevalent than type 1. It's characterized by a combination of insulin resistance and relative insulin deficiency. Insulin resistance means the body's cells don't respond effectively to insulin, preventing glucose from entering them. The pancreas initially tries to compensate by producing more insulin, but eventually, its capacity is overwhelmed, leading to a relative deficiency.
Characteristics: Type 2 diabetes typically develops gradually, often without noticeable symptoms in its early stages. Many individuals are diagnosed incidentally during routine blood tests. However, as the condition progresses, symptoms similar to type 1 diabetes may appear, including polyuria, polydipsia, polyphagia, and weight loss. However, the onset is slower and less dramatic.
Risk Factors: The primary risk factor for type 2 diabetes is obesity, particularly abdominal obesity. Other risk factors include family history, physical inactivity, unhealthy diet, and certain ethnicities (e.g., African American, Hispanic, Native American).
C. Gestational Diabetes: A Pregnancy-Related Challenge
Gestational diabetes is impaired glucose tolerance that develops during pregnancy. It typically resolves after delivery but carries a significant risk of developing type 2 diabetes later in life. The exact cause is unclear, but hormonal changes during pregnancy contribute to insulin resistance.
Characteristics: Symptoms may be similar to type 1 and type 2, but many women remain asymptomatic. Diagnosis is typically made through glucose tolerance tests during prenatal care.
Risk Factors: Obesity, family history of diabetes, and previous gestational diabetes are significant risk factors. Certain ethnicities are also at higher risk.
D. Other Specific Types: Rare but Significant
Several rare forms of diabetes fall outside the typical type 1 and type 2 categories. These include:
- Monogenic diabetes: Caused by genetic defects affecting insulin production or action.
- Pancreatic diabetes: Resulting from damage or disease of the pancreas (e.g., pancreatitis, cystic fibrosis).
- Cystic fibrosis-related diabetes: Diabetes often develops in individuals with cystic fibrosis.
- Drug-induced diabetes: Some medications can impair glucose metabolism and induce diabetes.
II. Complications of Diabetes Mellitus
Untreated or poorly managed diabetes can lead to a range of serious complications affecting various organs. These complications can significantly impair quality of life and increase mortality risk.
Macrovascular Complications: These affect large blood vessels and include:
- Cardiovascular disease: Heart disease (coronary artery disease, heart failure) and stroke are major causes of death in individuals with diabetes. High blood sugar damages blood vessels, increasing the risk of atherosclerosis (plaque buildup in arteries).
- Peripheral artery disease (PAD): Narrowing of the arteries in the legs and feet, leading to reduced blood flow and potentially limb amputation.
Microvascular Complications: These affect small blood vessels and include:
- Nephropathy (diabetic kidney disease): Damage to the kidneys, leading to kidney failure and requiring dialysis or kidney transplantation.
- Retinopathy (diabetic eye disease): Damage to the blood vessels in the retina, potentially leading to blindness.
- Neuropathy (diabetic nerve damage): Damage to nerves, resulting in numbness, tingling, pain, and reduced sensation, particularly in the feet and legs. This can increase the risk of foot ulcers and infections.
Other Complications:
- Foot ulcers: Due to neuropathy and reduced blood flow, minor injuries can easily become infected and lead to serious complications, including amputation.
- Infections: Individuals with diabetes are more susceptible to infections due to impaired immune function.
- Ketoacidosis: A life-threatening condition that occurs primarily in type 1 diabetes due to a severe lack of insulin. The body begins to break down fat for energy, producing ketones that accumulate in the blood, causing acidosis.
- Hyperosmolar hyperglycemic state (HHS): A severe complication primarily seen in type 2 diabetes, characterized by extremely high blood sugar levels and dehydration.
III. Management of Diabetes Mellitus
Effective diabetes management focuses on maintaining blood glucose levels within a target range to prevent or delay complications. The approach varies depending on the type of diabetes.
A. Type 1 Diabetes Management
Type 1 diabetes requires lifelong insulin therapy. This can be delivered through injections (using syringes or insulin pens) or an insulin pump. Careful blood glucose monitoring is essential to adjust insulin doses and maintain optimal control. Dietary management, including carbohydrate counting, is vital to regulate blood glucose levels. Regular physical activity is also crucial for overall health and improved insulin sensitivity.
B. Type 2 Diabetes Management
Type 2 diabetes management initially focuses on lifestyle modifications, including weight loss through diet and exercise. Oral hypoglycemic medications may be added if lifestyle changes are insufficient to control blood glucose. These medications work through different mechanisms, such as increasing insulin production, improving insulin sensitivity, or reducing glucose absorption. In some cases, insulin therapy may become necessary. Regular blood glucose monitoring, blood pressure monitoring, and lipid monitoring are essential.
C. Gestational Diabetes Management
Gestational diabetes is typically managed through dietary modifications and regular blood glucose monitoring. In some cases, insulin therapy may be required to maintain blood glucose levels within the target range. Regular prenatal checkups are crucial to monitor both maternal and fetal well-being.
D. Management of Other Specific Types
Management of other specific types of diabetes depends on the underlying cause and may involve specialized treatments. Genetic counseling and specific dietary considerations may be necessary.
IV. The Importance of Regular Monitoring and Follow-up
Regardless of the type of diabetes, regular monitoring and follow-up care are vital for successful management. This includes:
- Regular blood glucose monitoring: Frequency varies depending on individual needs and treatment regimen.
- Hemoglobin A1c (HbA1c) testing: Measures average blood glucose levels over the past 2-3 months.
- Blood pressure monitoring: To detect and manage hypertension.
- Lipid profile monitoring: To assess cholesterol and triglyceride levels.
- Regular check-ups with healthcare professionals: To monitor for complications and adjust treatment as needed.
- Foot care: Regular inspection of feet for cuts, blisters, or other problems. Proper foot care is crucial to prevent ulcers and infections.
- Eye exams: Annual eye exams are recommended to screen for diabetic retinopathy.
- Kidney function tests: Regular tests to assess kidney function and detect early signs of nephropathy.
This comprehensive guide aims to fill in the missing parts of the hypothetical table on diabetes mellitus, providing a detailed overview of its types, complications, and management. It is crucial to remember that diabetes management is a lifelong process requiring close collaboration between individuals with diabetes and their healthcare team. Early diagnosis and proactive management can significantly improve quality of life and reduce the risk of complications. Always consult with a healthcare professional for personalized advice and treatment.
Latest Posts
Latest Posts
-
Suppose That 650 Lb Of Coffee
Mar 25, 2025
-
Activity 1 1 Test Your Breakfast Food And Sandwiches Iq
Mar 25, 2025
-
A Guest Enjoying A Few Cocktails
Mar 25, 2025
-
Select All The Descriptions That Apply To The Rondo Form
Mar 25, 2025
-
Exploring Anatomy And Physiology In The Laboratory 4th Edition
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about Complete The Missing Parts Of The Table On Diabetes Mellitus . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
