Coronary Artery Disease Hesi Case Study
Onlines
Mar 19, 2025 · 6 min read
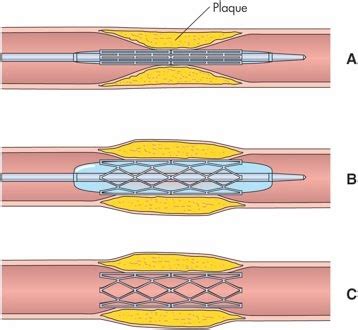
Table of Contents
Coronary Artery Disease: A Comprehensive HESI Case Study Analysis
Coronary artery disease (CAD), a leading cause of mortality globally, presents a complex clinical picture demanding thorough understanding and effective management. This article delves into a hypothetical HESI case study focusing on CAD, exploring its pathophysiology, clinical presentation, diagnostic approaches, treatment strategies, and nursing implications. We'll analyze a patient scenario, highlighting key assessment findings, interventions, and potential complications, emphasizing a holistic and evidence-based approach to care.
The Case Study: Mr. Jones's Journey
Mr. Jones, a 68-year-old Caucasian male with a history of smoking (30 pack-years), hypertension, and hyperlipidemia, presents to the emergency department (ED) complaining of chest pain. The pain began approximately 30 minutes ago, is described as a crushing pressure in his chest radiating to his left arm and jaw, and is associated with diaphoresis and shortness of breath. He denies any nausea or vomiting. His vital signs are: blood pressure (BP) 160/90 mmHg, heart rate (HR) 110 bpm, respiratory rate (RR) 24 breaths/min, oxygen saturation (SpO2) 90% on room air. An electrocardiogram (ECG) reveals ST-segment elevation in leads II, III, and aVF.
Pathophysiology of Coronary Artery Disease
Coronary artery disease, characterized by atherosclerosis of the coronary arteries, impairs blood flow to the myocardium. Atherosclerosis, a chronic inflammatory process, involves the buildup of plaque within arterial walls. This plaque, composed of cholesterol, lipids, inflammatory cells, and fibrous tissue, progressively narrows the artery lumen, reducing blood flow and oxygen delivery to the heart muscle. Risk factors, such as hypertension, hyperlipidemia, smoking, diabetes, obesity, and family history, accelerate this process.
Stages of Atherosclerosis:
- Endothelial Dysfunction: Damage to the endothelium, the inner lining of arteries, initiates the atherosclerotic process.
- Fatty Streak Formation: Lipids accumulate beneath the endothelium, forming fatty streaks.
- Plaque Formation: Fibrous tissue and inflammatory cells encapsulate the lipid deposits, forming atheromatous plaques.
- Plaque Rupture: Plaque rupture exposes thrombogenic material, triggering thrombus formation and potentially leading to acute coronary syndromes.
Clinical Manifestations of CAD
The clinical presentation of CAD is highly variable, ranging from asymptomatic disease to life-threatening events. Chest pain, or angina pectoris, is the hallmark symptom. Angina can manifest as:
- Stable Angina: Predictable chest pain typically occurring during exertion and relieved by rest or nitroglycerin.
- Unstable Angina: New-onset, worsening, or more frequent angina, indicating an increased risk of myocardial infarction (MI).
- Non-ST-Elevation Myocardial Infarction (NSTEMI): Partial blockage of a coronary artery, causing myocardial damage without significant ST-segment elevation on ECG.
- ST-Elevation Myocardial Infarction (STEMI): Complete blockage of a coronary artery, leading to significant myocardial damage and ST-segment elevation on ECG.
Mr. Jones's presentation strongly suggests an acute coronary syndrome (ACS), likely a STEMI given his ECG findings. Other symptoms such as diaphoresis, shortness of breath, and radiating pain are consistent with myocardial ischemia.
Diagnostic Evaluation of CAD
Prompt and accurate diagnosis is crucial in managing CAD. Key diagnostic tests include:
- Electrocardiogram (ECG): Detects myocardial ischemia or infarction based on characteristic changes in ST-segment and T-wave morphology.
- Cardiac Enzymes: Troponin I and T are highly specific markers of myocardial necrosis, indicating MI.
- Cardiac Catheterization: Invasive procedure providing visualization of coronary arteries and assessment of blood flow, enabling identification of blockages and their severity.
- Echocardiogram: Non-invasive imaging technique assessing cardiac structure and function, evaluating ventricular wall motion abnormalities and ejection fraction.
In Mr. Jones's case, the ECG demonstrating ST-segment elevation strongly supports the diagnosis of STEMI. Further investigations, including cardiac enzyme levels and cardiac catheterization, are essential to confirm the diagnosis and guide treatment.
Management of CAD
Management of CAD depends on the severity and presentation of the disease. Strategies include:
-
Medical Management: Medications play a pivotal role, encompassing:
- Antiplatelet agents (aspirin, clopidogrel): Inhibit platelet aggregation to prevent thrombus formation.
- Beta-blockers: Reduce myocardial oxygen demand and heart rate.
- Nitrates: Dilate coronary arteries and reduce myocardial oxygen demand.
- ACE inhibitors: Reduce blood pressure and improve cardiac remodeling.
- Statins: Lower cholesterol levels and reduce plaque formation.
-
Percutaneous Coronary Intervention (PCI): A minimally invasive procedure involving the insertion of a catheter to place a stent in the blocked coronary artery, restoring blood flow. This is the preferred treatment for STEMI.
-
Coronary Artery Bypass Grafting (CABG): Surgical procedure creating bypass grafts around blocked coronary arteries, improving blood flow to the myocardium. This may be indicated in cases where PCI is not feasible or successful.
In Mr. Jones's case, immediate PCI is indicated given the diagnosis of STEMI. This intervention aims to quickly restore blood flow to the affected myocardium, minimizing myocardial damage and improving prognosis.
Nursing Implications and Patient Care
Nursing care for a patient with CAD, particularly during an acute event like STEMI, is critical. Key nursing interventions include:
- Continuous ECG monitoring: To detect any arrhythmias or changes in myocardial ischemia.
- Vital sign monitoring: To assess hemodynamic stability and detect any deterioration.
- Oxygen therapy: To improve oxygenation and reduce myocardial oxygen demand.
- Pain management: Administering analgesics, such as morphine, to alleviate chest pain.
- Medication administration: Administering prescribed medications, including antiplatelet agents, beta-blockers, and nitrates, as ordered.
- Patient education: Providing comprehensive education regarding medication, lifestyle modifications, and follow-up care.
- Psychosocial support: Addressing the patient's anxiety and providing emotional support.
Post-PCI, careful monitoring for complications such as bleeding, hematoma formation, and restenosis is crucial. Long-term management includes lifestyle modifications, such as smoking cessation, dietary changes, regular exercise, and adherence to prescribed medications.
Potential Complications of CAD
Untreated or poorly managed CAD can lead to various complications, including:
- Myocardial Infarction (MI): Death of myocardial tissue due to prolonged ischemia.
- Heart Failure: Impaired ability of the heart to pump sufficient blood to meet the body's demands.
- Arrhythmias: Abnormal heart rhythms, potentially leading to sudden cardiac death.
- Cardiogenic Shock: Life-threatening condition where the heart fails to pump enough blood to meet the body's needs.
- Sudden Cardiac Death: Unexpected and abrupt cessation of cardiac function.
Continuous monitoring and prompt intervention are crucial to prevent or minimize these complications.
Long-Term Management and Prognosis
Long-term management of CAD focuses on risk factor modification and secondary prevention. This includes:
- Lifestyle changes: Smoking cessation, dietary modification (low-fat, low-sodium diet), regular exercise, weight management.
- Medication adherence: Consistent use of prescribed medications, such as antiplatelet agents, beta-blockers, statins, and ACE inhibitors.
- Cardiac rehabilitation: A supervised program encompassing exercise training, education, and psychosocial support.
- Regular follow-up appointments: To monitor disease progression and make necessary adjustments to treatment.
The prognosis for patients with CAD varies depending on factors such as the extent of coronary artery blockage, the presence of comorbidities, and the effectiveness of treatment. Early diagnosis, prompt intervention, and adherence to long-term management strategies significantly improve prognosis and reduce mortality risk.
Conclusion
This comprehensive analysis of a hypothetical HESI case study on coronary artery disease highlights the complexity of this prevalent cardiovascular condition. Understanding the pathophysiology, clinical presentation, diagnostic approaches, treatment strategies, and nursing implications is vital for effective management and improved patient outcomes. Emphasis on early detection, prompt intervention, and adherence to long-term management strategies is paramount in mitigating the risk of life-threatening complications and enhancing the prognosis for individuals affected by CAD. The case study underscores the importance of a multidisciplinary approach involving physicians, nurses, and other healthcare professionals in delivering holistic and patient-centered care. Continual learning and staying updated on the latest advancements in CAD management are crucial for healthcare professionals striving to provide optimal care for patients with this debilitating disease.
Latest Posts
Latest Posts
-
Geometry Unit 4 Congruent Triangles Quiz 4 1 Answer Key
Mar 20, 2025
-
Examples In History Of The Destructive Power Of Conformity
Mar 20, 2025
-
If You Are Charged With Selling Providing Delivering Alcohol Class A
Mar 20, 2025
-
Constitution And Bill Of Rights Scavenger Hunt Answer Key
Mar 20, 2025
-
You Have Recently Opened Your Own Internet Website Design
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about Coronary Artery Disease Hesi Case Study . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
