Diagnosis Reference Numbers Are Entered On The Cms-1500 Claim To
Onlines
Mar 24, 2025 · 6 min read
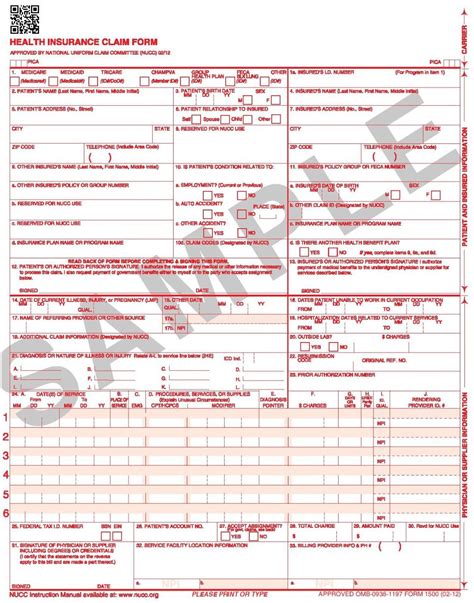
Table of Contents
Diagnosis Reference Numbers on the CMS-1500 Claim Form: A Comprehensive Guide
The CMS-1500 claim form, also known as the "HCFA-1500," is the standard paper claim form used by healthcare providers in the United States to bill insurance companies for medical services. Accurate completion of this form is crucial for timely and accurate reimbursement. One critical component of this process involves correctly entering the diagnosis reference numbers (DRGs). This article will delve into the importance, proper use, and potential pitfalls associated with entering DRGs on the CMS-1500 claim.
Understanding Diagnosis Codes and Their Significance
Before we dive into the specifics of entering DRGs on the CMS-1500, it's important to understand the fundamental role of diagnosis codes in medical billing. Diagnosis codes, primarily based on the International Classification of Diseases (ICD) system (currently ICD-10-CM in the US), are alphanumeric codes used to classify diseases, injuries, and other health conditions. These codes provide a standardized way for healthcare professionals to communicate about patient diagnoses, track disease prevalence, and analyze healthcare trends.
Why are accurate diagnosis codes crucial?
- Accurate Reimbursement: Insurance companies use diagnosis codes to determine medical necessity and the appropriate reimbursement amount. Incorrect or missing codes can lead to claim denials or reduced payments.
- Data Analysis and Public Health: Aggregated diagnosis data is used for epidemiological studies, public health surveillance, and resource allocation decisions. Accurate coding contributes to the reliability of this vital data.
- Compliance and Auditing: Proper use of diagnosis codes is essential for compliance with federal and state regulations. Audits frequently scrutinize this aspect of billing practices.
Locating the Diagnosis Reference Number Fields on the CMS-1500
The CMS-1500 form has designated fields for entering diagnosis codes. These are typically found in section 21 of the form. This section usually allows for up to four diagnosis codes to be reported. The exact location might vary slightly depending on the specific version of the form, but the general principle remains the same. It's imperative to consult the most current version of the CMS-1500 form for precise field locations.
The Process of Entering Diagnosis Reference Numbers
Entering DRGs correctly involves more than just transcribing the codes. It requires understanding the medical necessity of each code and ensuring its proper linkage to the procedures performed.
Step-by-step guide to accurate entry:
- Accurate Diagnosis: Begin by ensuring the correct diagnoses have been established by a qualified healthcare professional. The diagnosis should reflect the patient's condition as accurately as possible.
- ICD-10-CM Coding: Use the latest version of the ICD-10-CM coding manual to select the appropriate codes for the diagnosed conditions. This requires a thorough understanding of the coding conventions and guidelines.
- Medical Necessity: Verify that each reported diagnosis is directly related to the services provided and is medically necessary for the treatment rendered. Unrelated diagnoses should not be included.
- Sequencing of Codes: The primary diagnosis, the condition chiefly responsible for the patient's encounter, should be listed first. Subsequent diagnoses should be listed in order of importance. The sequencing must align with established medical practice guidelines.
- Completeness and Clarity: Ensure that all required fields are completed accurately and legibly. Any errors or inconsistencies can delay processing and lead to denials.
- Verification: Before submitting the claim, carefully review all entered information, including the diagnosis codes, to ensure accuracy and completeness.
Common Mistakes and How to Avoid Them
Numerous errors can occur when entering DRGs on the CMS-1500 form. Understanding common mistakes is crucial for preventing claim denials and ensuring timely reimbursement.
1. Incorrect Code Selection: Using outdated codes, incorrectly interpreting code descriptions, or failing to select the most specific code can result in denials. Always consult the latest ICD-10-CM manual and seek clarification when needed.
2. Missing Codes: Failing to include necessary diagnoses or neglecting to list the primary diagnosis can hinder the claim processing. Ensure all relevant diagnoses are listed in the designated fields.
3. Incorrect Sequencing of Codes: Improper sequencing of diagnoses can cause confusion and lead to payment issues. Always list the primary diagnosis first, followed by secondary diagnoses in order of importance.
4. Inconsistent Coding: Using inconsistent codes across different claims or for the same patient can raise red flags and lead to audits. Maintain consistency in your coding practices.
5. Lack of Medical Necessity: Including diagnoses that are not directly related to the services rendered is a serious error. All diagnoses should directly support the medical necessity of the services billed.
6. Illegible or Incomplete Entries: Unclear or incomplete entries make it difficult for insurance companies to process the claim and often result in denials or delays. Ensure that all entries are legible and complete.
7. Using Placeholder Codes: Using placeholder codes (codes used temporarily while the correct code is being determined) should be avoided. Only enter confirmed and accurate codes.
Impact of Incorrect DRGs on Claim Processing
Incorrectly entered DRGs can have far-reaching implications, including:
- Claim Denials: Incorrect or missing codes are the leading cause of claim denials. This can result in significant financial losses for healthcare providers.
- Delayed Payments: Even if not denied outright, claims with errors may experience significant delays in processing. This can disrupt cash flow and negatively impact practice finances.
- Audits and Investigations: Frequent or significant coding errors can trigger audits and investigations by insurance payers or government agencies.
- Reputational Damage: Frequent claim denials due to coding errors can damage a healthcare provider’s reputation and potentially affect patient referrals.
- Financial Penalties: In some cases, intentional or recurrent coding errors can result in financial penalties and sanctions.
Strategies for Improving Accuracy
Improving accuracy in entering DRGs requires a multifaceted approach, including:
- Invest in Training: Provide comprehensive training to billing staff on proper ICD-10-CM coding, CMS-1500 form completion, and medical billing regulations.
- Implement Quality Control Measures: Establish robust quality control procedures to review claims before submission. Regular audits of coding practices are essential.
- Utilize Coding Software: Invest in electronic health record (EHR) systems and medical billing software that incorporates automated coding tools and validation checks.
- Stay Updated: Keep abreast of changes and updates to the ICD-10-CM coding system and CMS-1500 form requirements. Subscribe to relevant publications and participate in continuing education programs.
- Seek Expert Advice: Consult with a qualified medical coder or billing specialist when uncertain about appropriate codes or encounter complex cases.
- Regular Audits: Perform internal audits to identify and correct any deficiencies in coding and billing practices.
Conclusion
Entering diagnosis reference numbers accurately on the CMS-1500 claim form is vital for timely and accurate reimbursement. Understanding the importance of accurate coding, employing proper procedures, and implementing effective quality control measures are essential for optimizing the billing process and ensuring financial success. By following the guidelines presented in this article and staying proactive in updating knowledge and procedures, healthcare providers can significantly reduce the risk of claim denials, improve efficiency, and enhance their overall financial health. The potential financial and reputational consequences of errors underscore the critical need for continuous improvement and attention to detail in this crucial aspect of medical billing. Investing time and resources into training, technology, and quality control procedures will ultimately yield substantial returns in the form of improved claim processing, reduced denials, and strengthened financial stability.
Latest Posts
Latest Posts
-
Math 1314 Lab Module 3 Answers
Mar 28, 2025
-
Rate Of Return Chapter 3 Lesson 6
Mar 28, 2025
-
Ap Csa Unit 4 Progress Check Mcq
Mar 28, 2025
-
Baked Dessert Into Garden Tool Puzzle
Mar 28, 2025
-
Quotes From Everything I Never Told You
Mar 28, 2025
Related Post
Thank you for visiting our website which covers about Diagnosis Reference Numbers Are Entered On The Cms-1500 Claim To . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
