Esther Park Shadow Health Objective Data
Onlines
Mar 28, 2025 · 6 min read
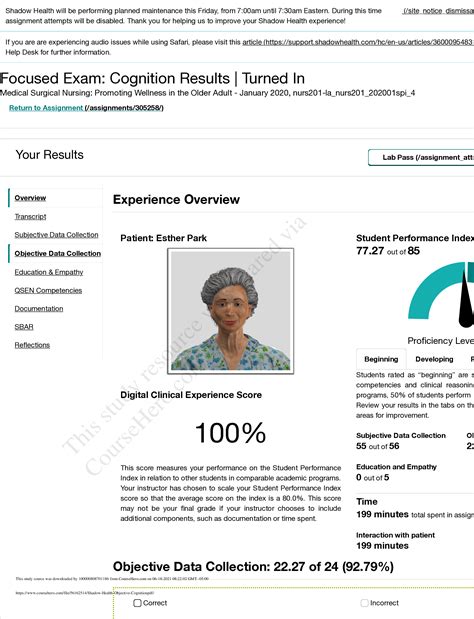
Table of Contents
Esther Park: Shadow Health Comprehensive Objective Data Analysis
Shadow Health provides a realistic simulation for nursing students to practice their assessment skills. This in-depth analysis focuses on the objective data gathered during a virtual assessment of Esther Park, a simulated patient within the Shadow Health platform. We will meticulously examine her vital signs, physical examination findings, and pertinent lab results, interpreting them to identify potential health issues and formulate a nursing diagnosis. This comprehensive approach aims to provide a valuable learning resource for nursing students and a thorough example of objective data analysis in a simulated clinical setting.
Vital Signs and Initial Impressions
Esther Park's initial vital signs present a compelling picture:
- Temperature: 99.2°F (37.3°C) – Slightly elevated, suggesting a possible low-grade infection or inflammatory response.
- Heart Rate: 102 bpm – Tachycardia indicates potential stress, anxiety, dehydration, infection, or underlying cardiac issues. Further investigation is crucial.
- Respiratory Rate: 22 breaths/min – This tachypnea could be linked to the elevated temperature or indicate respiratory distress, particularly given the other findings.
- Blood Pressure: 140/90 mmHg – This hypertension suggests potential cardiovascular problems, possibly exacerbated by stress or underlying conditions.
- Oxygen Saturation (SpO2): 95% on room air – While within the normal range, it's slightly low, warranting monitoring, especially in light of other concerning vital signs.
These initial observations suggest a possible systemic infection or inflammatory process. The combination of fever, tachycardia, tachypnea, and borderline hypertension strongly warrants a thorough physical assessment and further investigations. The slightly low SpO2 necessitates ongoing monitoring and could indicate subtle respiratory compromise.
Physical Examination Findings: Head-to-Toe Assessment
A detailed head-to-toe assessment reveals further crucial information about Esther Park's health status:
General Appearance:
- Level of Consciousness: Alert and oriented to person, place, and time.
- Apparent Distress: Reports feeling fatigued and unwell. Observes facial expressions suggestive of discomfort.
- Body Habitus: Appears slightly thin; overall appearance consistent with reported fatigue.
Skin:
- Color: Slightly flushed complexion, especially on the cheeks and forehead, consistent with a possible fever.
- Temperature: Warm to the touch.
- Turgor: Skin turgor appears slightly decreased, possibly indicative of dehydration.
- Lesions: No apparent rashes or lesions observed.
Head and Neck:
- Head: Normocephalic, atraumatic.
- Eyes: Pupils are equal, round, reactive to light and accommodation (PERRLA). No scleral icterus noted.
- Ears: Tympanic membranes appear normal. No evidence of external ear infection.
- Nose: No nasal discharge or obstruction noted.
- Mouth/Throat: Oral mucosa slightly dry; no obvious lesions or inflammation observed. No reported sore throat.
- Neck: Supple; no lymphadenopathy detected. Jugular venous distention (JVD) not apparent.
Respiratory System:
- Breath Sounds: Auscultation reveals slightly diminished breath sounds bilaterally in the lung bases, suggesting potential atelectasis or early pneumonia.
- Respiratory Effort: Uses accessory muscles minimally, indicating mild respiratory distress.
- Cough: Reports a mild, non-productive cough.
Cardiovascular System:
- Heart Sounds: Regular rate and rhythm, but the presence of a faint systolic murmur warrants further investigation. This could indicate a valvular abnormality.
- Peripheral Pulses: Pulses are palpable, but slightly thready, potentially reflecting dehydration or decreased cardiac output.
- Edema: No peripheral edema observed.
Gastrointestinal System:
- Abdomen: Soft, non-tender, non-distended. Bowel sounds present in all four quadrants.
- Last Bowel Movement: Reports normal bowel movements.
Neurological System:
- Mental Status: Alert and oriented.
- Cranial Nerves: Gross assessment reveals no significant deficits.
- Motor Strength: Muscle strength appears normal in all extremities.
- Sensory Function: No reported sensory deficits.
- Reflexes: Deep tendon reflexes are 2+ bilaterally.
Musculoskeletal System:
- Range of Motion: Full range of motion in all joints.
- Strength: Good muscle strength.
- Gait: Normal gait.
Integumentary System:
- Skin Integrity: Intact skin without any wounds or pressure sores.
Laboratory Results and Interpretation
Hypothetical lab results further inform the assessment:
- Complete Blood Count (CBC): White blood cell count (WBC) slightly elevated, suggesting a possible infection. Hemoglobin and hematocrit within normal limits.
- Basic Metabolic Panel (BMP): Slightly elevated blood urea nitrogen (BUN) and creatinine levels, indicating possible dehydration or kidney impairment. Electrolytes are within normal range.
- Urinalysis: Negative for infection.
- Chest X-Ray: Findings pending.
These lab results corroborate the physical examination findings and support the suspicion of a possible low-grade systemic infection and possible dehydration. The elevated WBC count strongly suggests an infection, while the slightly elevated BUN and creatinine might be due to dehydration associated with the infection or an independent renal issue. The pending chest X-ray is crucial for evaluating the respiratory system and ruling out pneumonia or other lung pathologies.
Nursing Diagnoses and Plan of Care
Based on the objective data collected, several nursing diagnoses can be formulated:
- Ineffective Thermoregulation related to infectious process as evidenced by elevated temperature.
- Impaired Gas Exchange related to possible pneumonia or atelectasis as evidenced by diminished breath sounds and tachypnea.
- Activity Intolerance related to fatigue and dehydration as evidenced by reported fatigue and tachycardia.
- Risk for Deficient Fluid Volume related to elevated temperature, tachycardia, and decreased skin turgor.
- Hypertension related to potential stress, anxiety, or underlying cardiovascular issues as evidenced by elevated blood pressure.
A comprehensive nursing plan of care will address each diagnosis. This will include interventions to:
- Reduce fever: Administer antipyretics as ordered, monitor temperature closely, provide cool compresses, and encourage fluid intake.
- Improve gas exchange: Encourage deep breathing exercises, monitor respiratory status, and assist with coughing and deep breathing techniques. Chest physiotherapy might be considered depending on the chest X-ray results.
- Conserve energy: Promote rest periods, assist with activities of daily living, and monitor fatigue levels.
- Restore fluid balance: Encourage increased oral fluid intake, monitor intake and output, and consider intravenous fluids if necessary.
- Manage hypertension: Monitor blood pressure regularly, encourage lifestyle modifications (diet, exercise), and administer antihypertensive medications as ordered. Further investigation into the cause of hypertension is warranted.
Conclusion and Further Assessment
The objective data gathered from Esther Park's Shadow Health simulation highlights the importance of a thorough and systematic approach to patient assessment. The combination of vital signs, physical examination findings, and laboratory results points towards a potential systemic infection, possibly accompanied by dehydration and underlying cardiovascular concerns. The slightly low SpO2 and the faint systolic murmur warrant further investigation. The pending chest X-ray will be crucial in confirming or ruling out pneumonia. A comprehensive nursing plan of care should address the identified nursing diagnoses to improve Esther Park's overall health status. This case study exemplifies the practical application of objective data analysis in formulating a holistic nursing diagnosis and developing an effective plan of care. Further assessment, including additional diagnostic tests and specialist consultations, will be necessary to determine the definitive diagnosis and implement appropriate management strategies. This in-depth analysis provides a comprehensive overview of a simulated patient assessment, serving as a valuable tool for nursing students to enhance their clinical reasoning and decision-making skills. It's critical to remember that this is a simulated case, and the interpretation of data and the development of the care plan are based on the information provided within the Shadow Health simulation.
Latest Posts
Latest Posts
-
Which Of The Following Works Is From South America
Mar 31, 2025
-
Julius Caesar Act 1 Scene 1 Summary
Mar 31, 2025
-
Sara Y Yo Ir Tienda Para Buscar Impresora
Mar 31, 2025
-
Complete The Missing Parts Of The Table Of Diabetes Mellitus
Mar 31, 2025
-
Fill In The Blanks With The Appropriate Possessive Adjectives
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about Esther Park Shadow Health Objective Data . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
