Heart Failure With Atrial Fibrillation Hesi Case Study
Onlines
Mar 13, 2025 · 7 min read
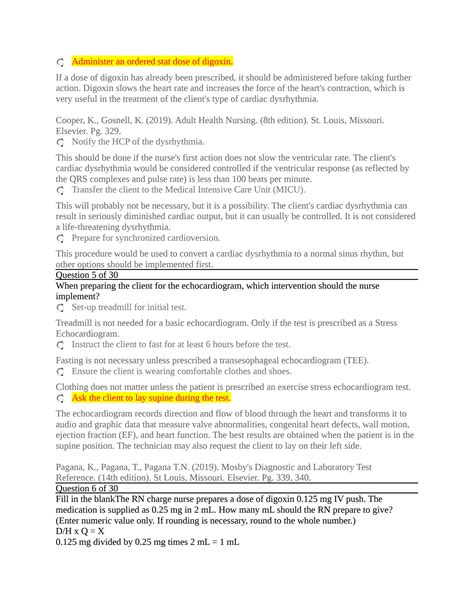
Table of Contents
Heart Failure with Atrial Fibrillation: A Comprehensive HESI Case Study Analysis
Heart failure (HF) coupled with atrial fibrillation (AFib) presents a complex clinical scenario demanding a multifaceted approach to patient management. This article delves into a hypothetical HESI case study focusing on a patient experiencing this dual diagnosis, exploring the pathophysiology, assessment findings, nursing interventions, and potential complications. We will analyze the case through the lens of evidence-based practice, emphasizing the importance of collaborative care and patient education.
Understanding the Pathophysiology: Heart Failure and Atrial Fibrillation
Before examining the case study, let's establish a foundational understanding of both heart failure and atrial fibrillation and how their coexistence exacerbates the clinical picture.
Heart Failure (HF)
Heart failure is a clinical syndrome characterized by the heart's inability to pump sufficient blood to meet the body's metabolic demands. This leads to a cascade of events, including fluid overload, reduced tissue perfusion, and activation of neurohormonal systems. The underlying causes are diverse, ranging from coronary artery disease (CAD), hypertension, valvular heart disease, and cardiomyopathies to congenital heart defects. HF is broadly categorized into two main types:
-
Heart Failure with reduced ejection fraction (HFrEF): Characterized by weakened heart muscle resulting in reduced ability to pump blood effectively. The ejection fraction (EF), which represents the percentage of blood ejected from the left ventricle with each contraction, is typically below 40%.
-
Heart Failure with preserved ejection fraction (HFpEF): In this type, the heart muscle's ability to relax and fill with blood is impaired, despite a relatively normal ejection fraction. This often affects older adults and is frequently associated with hypertension and diastolic dysfunction.
Atrial Fibrillation (AFib)
Atrial fibrillation is the most common sustained cardiac arrhythmia. It's characterized by rapid, irregular atrial contractions, disrupting the normal coordinated electrical activity of the heart. This chaotic electrical activity results in:
- Inefficient atrial emptying: Leading to reduced cardiac output and potentially contributing to heart failure.
- Increased risk of thromboembolism: The stagnant blood in the atria can form clots, increasing the risk of stroke.
- Increased workload on the ventricles: The rapid, irregular atrial impulses can lead to ventricular tachycardia or other potentially fatal arrhythmias.
The Combined Impact of HF and AFib
The coexistence of HF and AFib significantly worsens the prognosis. AFib exacerbates the symptoms of HF by reducing cardiac output, increasing pulmonary congestion, and promoting thrombus formation. Conversely, HF can predispose to AFib due to left atrial dilation and myocardial dysfunction. This complex interplay demands a comprehensive assessment and management strategy.
The Hypothetical HESI Case Study: Mrs. Jones
Patient: Mrs. Jones, a 72-year-old female with a history of hypertension, coronary artery disease (CAD), and type 2 diabetes mellitus (T2DM).
Presenting Complaint: Shortness of breath (dyspnea) on exertion, worsening over the past three months, accompanied by paroxysmal nocturnal dyspnea (PND) and lower extremity edema.
Assessment Findings:
- Vital Signs: Blood pressure 160/90 mmHg, heart rate 120 bpm and irregularly irregular, respiratory rate 24 breaths/min, oxygen saturation 88% on room air.
- Cardiac Exam: Tachycardia, irregular rhythm, S3 gallop present, diminished breath sounds at the bases.
- Pulmonary Exam: Crackles bilaterally, especially at the bases.
- Peripheral Exam: 2+ pitting edema in both lower extremities.
- Electrocardiogram (ECG): Atrial fibrillation with a rapid ventricular response.
- Chest X-ray: Cardiomegaly, pulmonary edema.
- Laboratory Values: Elevated BNP (B-type natriuretic peptide), elevated creatinine, slightly elevated potassium levels.
Nursing Interventions: Prioritizing Patient Care
Based on Mrs. Jones's presentation, the nursing interventions should prioritize stabilizing her hemodynamic status, managing her symptoms, and preventing complications. These interventions should be guided by the following principles:
1. Airway, Breathing, Circulation (ABCs):
- Oxygen Therapy: Immediate administration of supplemental oxygen to improve oxygen saturation. Titration of oxygen flow rate is essential to achieve optimal oxygenation without causing oxygen toxicity.
- Fluid Management: Careful monitoring of fluid balance, including intake and output (I&O). Diuretics may be administered to reduce pulmonary congestion and edema. Close monitoring of electrolyte levels, particularly potassium, is crucial.
- Hemodynamic Monitoring: Continuous monitoring of heart rate, blood pressure, and oxygen saturation. If indicated, invasive hemodynamic monitoring (e.g., pulmonary artery catheter) may be used to assess cardiac function and guide fluid management.
2. Rate Control and Rhythm Management:
- Medication Administration: Beta-blockers, calcium channel blockers, or digoxin might be used to control the ventricular rate in AFib. The choice depends on the patient's overall health and other medications. Antiarrhythmic drugs might be considered to restore sinus rhythm but carry potential risks.
- Cardioversion: If rate control is ineffective and the patient is hemodynamically unstable, cardioversion (either electrical or pharmacological) might be necessary to restore normal sinus rhythm.
3. Thromboembolism Prevention:
- Anticoagulation: Due to the risk of stroke, anticoagulation therapy is critical. The choice of anticoagulant (warfarin, direct thrombin inhibitors, or factor Xa inhibitors) will depend on the patient's individual risk factors and other medical conditions. Regular monitoring of INR (international normalized ratio) or other relevant coagulation parameters is required.
4. Symptom Management:
- Pain Management: Assessment and management of any chest pain or discomfort using appropriate analgesics.
- Dyspnea Management: Positioning the patient for optimal breathing, providing emotional support, and considering non-invasive ventilation if dyspnea is severe.
- Edema Management: Elevate the lower extremities to reduce edema and improve venous return.
5. Patient Education and Support:
- Medication Education: Thorough education on the purpose, dosage, side effects, and potential interactions of all prescribed medications.
- Lifestyle Modifications: Guidance on lifestyle changes, such as dietary restrictions (sodium and fluid restriction), regular exercise (as tolerated), and stress management techniques.
- Disease Management: Comprehensive education about heart failure and atrial fibrillation, including symptom recognition and management.
- Emotional Support: Addressing the patient's emotional and psychological needs, offering emotional support, and encouraging adherence to the treatment plan.
Potential Complications and Their Management
Several complications can arise in patients with HF and AFib, requiring prompt intervention:
- Stroke: The most serious complication due to the increased risk of thrombus formation. Prevention through anticoagulation is crucial. Rapid recognition and management of stroke symptoms are essential.
- Pulmonary Edema: Fluid accumulation in the lungs, causing severe shortness of breath. Treatment involves oxygen therapy, diuretics, and potentially non-invasive or invasive ventilation.
- Cardiogenic Shock: The heart's inability to pump enough blood to meet the body's needs, leading to organ dysfunction. Requires aggressive hemodynamic support and potentially inotropic medications.
- Heart Failure Exacerbation: Worsening of heart failure symptoms, requiring adjustments in medication, fluid management, and potentially hospitalization.
- Electrolyte Imbalances: Potassium and magnesium imbalances are common, particularly with diuretic use. Close monitoring and correction are necessary to prevent potentially fatal arrhythmias.
Collaborative Care: The Multidisciplinary Team Approach
Managing patients with HF and AFib requires a collaborative approach involving a multidisciplinary team:
- Cardiologist: Provides specialized expertise in cardiac diagnosis and management.
- Nurse Practitioner or Physician Assistant: Assists in patient assessment, medication management, and education.
- Registered Nurse: Provides direct patient care, monitoring vital signs, administering medications, and educating the patient and family.
- Pharmacist: Ensures medication safety and efficacy, addresses potential drug interactions, and provides patient counseling.
- Respiratory Therapist: Provides respiratory support, including oxygen therapy, and management of respiratory complications.
- Dietitian: Provides dietary counseling and guidance on sodium and fluid restriction.
- Physical Therapist: Develops a tailored exercise program to improve cardiac function and overall fitness.
- Social Worker: Provides psychosocial support, addresses social determinants of health, and assists with discharge planning.
Conclusion: Holistic Approach to Optimal Outcomes
Managing heart failure with atrial fibrillation requires a comprehensive and integrated approach. Careful assessment, timely interventions, and close collaboration among healthcare professionals are crucial for optimizing patient outcomes. The focus should not only be on managing acute symptoms but also on preventing complications, improving quality of life, and enhancing patient education to promote long-term self-management and adherence to treatment plans. This holistic approach ensures that patients with this complex condition receive the best possible care and achieve the highest possible level of functional capacity and quality of life.
Latest Posts
Latest Posts
-
Infer Geologic History From A New Mexico Outcrop
Mar 14, 2025
-
For Whom The Bell Tolls Summary
Mar 14, 2025
-
The Last Time I Bought This Product It Cost 20 00
Mar 14, 2025
-
How Can An Operation Assist Customers With Food Allergies
Mar 14, 2025
-
Chapter 3 Of Animal Farm Summary
Mar 14, 2025
Related Post
Thank you for visiting our website which covers about Heart Failure With Atrial Fibrillation Hesi Case Study . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
