Hesi Case Studies Heart Failure With Atrial Fibrillation
Onlines
Mar 13, 2025 · 6 min read
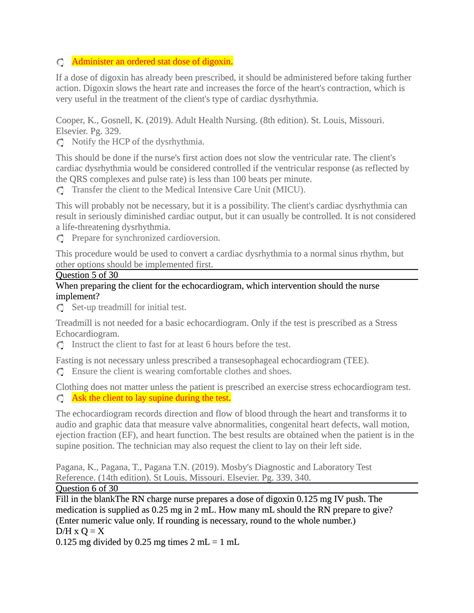
Table of Contents
HESIs Case Studies: Heart Failure with Atrial Fibrillation – A Comprehensive Guide
Heart failure (HF) and atrial fibrillation (AFib) are common cardiovascular conditions often presenting concurrently, significantly increasing morbidity and mortality. Understanding their pathophysiology, clinical presentation, and management is crucial for healthcare professionals. This article delves into HESIs case studies focusing on heart failure with atrial fibrillation, providing a comprehensive overview to aid in improved patient care and exam preparation.
Understanding Heart Failure and Atrial Fibrillation
Before examining specific case studies, let's establish a foundational understanding of both conditions:
Heart Failure (HF)
Heart failure, also known as congestive heart failure, is a clinical syndrome characterized by the heart's inability to pump sufficient blood to meet the body's metabolic demands. This leads to fluid buildup (congestion) and reduced tissue perfusion. Several factors contribute to HF, including:
- Reduced contractility: The heart muscle weakens, reducing its ability to pump effectively.
- Increased afterload: Resistance against which the heart must pump increases (e.g., due to hypertension).
- Increased preload: Increased volume returning to the heart stretches the heart muscle beyond its optimal length.
- Valve dysfunction: Problems with heart valves can impede blood flow.
Types of Heart Failure:
- Systolic Heart Failure: Impaired ability of the heart to contract and eject blood.
- Diastolic Heart Failure: Impaired ability of the heart to relax and fill with blood.
Clinical Manifestations of Heart Failure:
- Shortness of breath (dyspnea): Often exacerbated by exertion (exertional dyspnea) or lying down (orthopnea).
- Fatigue and weakness: Due to reduced oxygen delivery to tissues.
- Edema: Fluid accumulation in the extremities (peripheral edema), lungs (pulmonary edema), or abdomen (ascites).
- Cough: Often productive with pink, frothy sputum in pulmonary edema.
- Tachycardia: Rapid heart rate as the heart attempts to compensate.
- Weight gain: Due to fluid retention.
Atrial Fibrillation (AFib)
Atrial fibrillation is an irregular and often rapid heart rhythm originating from abnormal electrical signals in the atria. This leads to chaotic atrial activity, inefficient atrial contraction, and potentially rapid ventricular rates. Key features of AFib include:
- Irregularly irregular pulse: The heartbeat is unpredictable and varies in rhythm.
- Palpitations: Awareness of a rapid or irregular heartbeat.
- Shortness of breath (dyspnea): Due to reduced cardiac output and potential pulmonary congestion.
- Fatigue and weakness: Similar to HF, due to reduced tissue perfusion.
- Dizziness or lightheadedness: From reduced cerebral blood flow.
- Chest pain (angina): In some cases, due to increased myocardial oxygen demand.
Risk Factors for Atrial Fibrillation:
- Age: Risk increases significantly with age.
- Hypertension: High blood pressure damages heart structures.
- Heart valve disease: Structural abnormalities disrupt normal electrical conduction.
- Congenital heart defects: Birth defects affecting heart structure.
- Thyroid disorders: Hormonal imbalances affect heart rhythm.
- Alcohol abuse: Can trigger AFib episodes.
- Sleep apnea: Intermittent hypoxia stresses the cardiovascular system.
- Diabetes: Associated with increased risk of cardiovascular complications.
- Obesity: Increases the workload on the heart.
- Family history: Genetic predisposition to arrhythmias.
Heart Failure with Atrial Fibrillation: A Synergistic Relationship
The coexistence of heart failure and atrial fibrillation creates a complex clinical scenario. AFib can exacerbate heart failure by several mechanisms:
- Reduced cardiac output: Inefficient atrial contraction reduces the amount of blood delivered to the ventricles, further compromising cardiac output.
- Increased risk of thromboembolism: The stagnant blood in the atria increases the risk of clot formation, leading to stroke or pulmonary embolism.
- Increased heart rate: Rapid ventricular rates increase myocardial oxygen demand, worsening symptoms of heart failure.
- Pro-inflammatory effects: AFib is associated with systemic inflammation, further damaging the already compromised heart muscle.
Conversely, heart failure can contribute to the development of atrial fibrillation through:
- Myocardial remodeling: Changes in heart structure and function can lead to electrical abnormalities.
- Neurohormonal activation: Increased levels of hormones like norepinephrine can increase the risk of arrhythmias.
- Increased atrial pressure: Elevated pressure in the atria predisposes to electrical instability.
HESIs Case Studies: Analyzing Clinical Scenarios
Let's now explore some hypothetical HESIs case studies highlighting heart failure with atrial fibrillation. Each case will focus on specific clinical presentations, diagnostic approaches, and treatment strategies.
Case Study 1: The Elderly Patient with Progressive Dyspnea
A 78-year-old female presents with progressive shortness of breath over the past three months. She reports increasing fatigue, orthopnea, and paroxysmal nocturnal dyspnea. Physical examination reveals bilateral crackles in the lung bases, jugular venous distension (JVD), and pitting edema in her lower extremities. Her ECG shows atrial fibrillation with a rapid ventricular response. Echocardiography reveals reduced ejection fraction (EF) and mild mitral regurgitation.
Key Considerations:
- Diagnosis: Heart failure with reduced ejection fraction (HFrEF) and atrial fibrillation.
- Treatment: Management involves rate control of AFib (e.g., beta-blockers, digoxin), rhythm control (e.g., cardioversion, antiarrhythmic drugs), and HF management (e.g., ACE inhibitors, beta-blockers, diuretics). Anticoagulation (e.g., warfarin, direct oral anticoagulants) is crucial to prevent thromboembolic events.
Case Study 2: The Patient with Sudden-Onset Shortness of Breath and Chest Pain
A 65-year-old male with a history of hypertension and heart failure presents to the emergency department with sudden-onset shortness of breath and chest pain. He reports feeling palpitations prior to the onset of symptoms. His ECG reveals atrial fibrillation with a rapid ventricular rate. His blood pressure is low, and he is tachypneic and diaphoretic.
Key Considerations:
- Differential Diagnosis: Acute pulmonary edema, acute coronary syndrome, or acute decompensated heart failure.
- Treatment: Requires urgent assessment and stabilization. Treatment may include oxygen therapy, intravenous diuretics, and potentially inotropic support. Rapid rate control and anticoagulation are essential. Further investigation, such as cardiac biomarkers and coronary angiography, may be necessary.
Case Study 3: The Asymptomatic Patient with Incidentally Discovered Atrial Fibrillation
A 60-year-old male undergoes a routine physical examination. His ECG reveals atrial fibrillation with a normal ventricular rate. He is asymptomatic and denies any symptoms of heart failure. His echocardiogram shows a preserved ejection fraction.
Key Considerations:
- Management: Even in asymptomatic patients, AFib requires close monitoring and treatment to prevent complications. Anticoagulation is usually recommended to reduce the risk of stroke. Regular follow-up is necessary to detect any potential development of symptoms.
Nursing Considerations in Managing Heart Failure with Atrial Fibrillation
Nursing care plays a vital role in managing patients with heart failure and atrial fibrillation. Key nursing interventions include:
- Monitoring vital signs: Closely monitoring heart rate, blood pressure, respiratory rate, and oxygen saturation.
- Assessing fluid status: Monitoring daily weights, intake and output, and signs of edema.
- Administering medications: Accurately administering prescribed medications and monitoring for adverse effects.
- Providing patient education: Educating patients about their condition, medications, and lifestyle modifications.
- Promoting activity and rest: Balancing rest with appropriate activity to improve cardiac function and prevent deconditioning.
- Monitoring for complications: Closely monitoring for signs of pulmonary edema, hypotension, and thromboembolic events.
Lifestyle Modifications and Patient Education
Lifestyle modifications are crucial for managing heart failure with atrial fibrillation. Educating patients on the following is paramount:
- Dietary changes: Reducing sodium intake, limiting fluid intake, and following a heart-healthy diet.
- Activity modification: Engaging in regular, moderate exercise as tolerated.
- Weight management: Achieving and maintaining a healthy weight.
- Smoking cessation: Smoking significantly worsens cardiovascular health.
- Alcohol moderation: Excessive alcohol consumption can trigger AFib episodes.
- Stress management: Stress can negatively impact cardiovascular function.
Conclusion
Heart failure with atrial fibrillation presents a significant clinical challenge requiring a comprehensive and multidisciplinary approach. Understanding the pathophysiology, clinical manifestations, and management strategies of both conditions is essential for healthcare professionals. This article has explored several hypothetical HESIs case studies to illustrate the complexity of this clinical scenario and the importance of prompt diagnosis and effective management to improve patient outcomes and prepare for examinations effectively. Remember that this information is for educational purposes and should not be considered medical advice. Always consult with qualified healthcare professionals for diagnosis and treatment.
Latest Posts
Latest Posts
-
Characters In 2001 A Space Odyssey
Mar 14, 2025
-
Summary Chapter 1 Things Fall Apart
Mar 14, 2025
-
What Did The Spanish Farmer Say To His Chicken
Mar 14, 2025
-
Aerial Photographs Satellite Images And Topographic Maps Lab Report 7
Mar 14, 2025
-
Separation Career Development Boards Are Held At What Level
Mar 14, 2025
Related Post
Thank you for visiting our website which covers about Hesi Case Studies Heart Failure With Atrial Fibrillation . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
