Hesi Case Study Benign Prostatic Hyperplasia
Onlines
Mar 14, 2025 · 7 min read
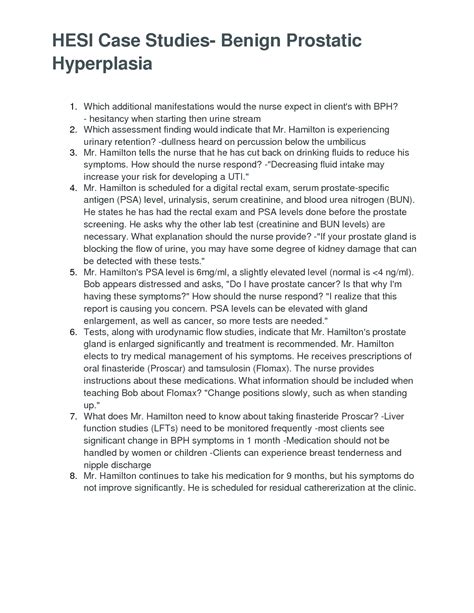
Table of Contents
HES Case Study: Benign Prostatic Hyperplasia (BPH) – A Comprehensive Analysis
Benign prostatic hyperplasia (BPH), also known as prostate gland enlargement, is a common condition affecting men as they age. This case study will delve into the complexities of BPH, exploring its pathophysiology, clinical presentation, diagnostic approaches, and management strategies, drawing from a hypothetical HES (Health Education Systems, Inc.) scenario. We will analyze a patient's journey, highlighting key decision points and emphasizing the importance of holistic care. This in-depth analysis will provide a comprehensive understanding of BPH for healthcare professionals and students.
Understanding Benign Prostatic Hyperplasia (BPH)
BPH is characterized by the non-cancerous enlargement of the prostate gland, a walnut-sized organ located below the bladder. This enlargement can obstruct the urethra, leading to a range of lower urinary tract symptoms (LUTS). The exact etiology remains unclear, but hormonal changes, particularly the interaction of dihydrotestosterone (DHT) and estrogen, are believed to play a significant role. As men age, DHT stimulates prostate cell growth, leading to gradual enlargement.
Pathophysiology of BPH:
The pathophysiological mechanisms underlying BPH are complex and multifaceted, involving:
- Hormonal Imbalance: An imbalance between androgens (like DHT) and estrogens is strongly implicated. Elevated DHT levels stimulate prostate cell proliferation, while decreased androgen/estrogen ratio may also contribute.
- Cellular Proliferation: BPH is characterized by an increased rate of cellular proliferation in the prostate gland, leading to its enlargement.
- Stromal and Epithelial Cell Growth: Both stromal (supportive tissue) and epithelial cells contribute to the overall increase in prostate volume.
- Urethral Compression: The enlarged prostate gland compresses the urethra, leading to the characteristic urinary symptoms of BPH.
Clinical Presentation of BPH:
The clinical presentation of BPH is highly variable, with symptoms ranging from mild inconvenience to severe disability. The most common symptoms fall under the category of LUTS and can include:
- Storage Symptoms: These relate to bladder filling and include frequency (urinating often), urgency (sudden, strong urge to urinate), nocturia (waking up at night to urinate), and urge incontinence (leaking urine due to strong urge).
- Voiding Symptoms: These relate to the process of emptying the bladder and include hesitancy (difficulty starting urination), weak stream, intermittent stream (stopping and starting), straining to urinate, and terminal dribbling (leakage after urination).
- Post-Micturition Symptoms: These symptoms occur after urination and include a sensation of incomplete bladder emptying.
Severity of symptoms: The severity of BPH symptoms varies significantly among individuals. Some men may experience minimal discomfort, while others may suffer debilitating symptoms that severely impact their quality of life.
The HES Case Study: Mr. Jones
Let's consider a hypothetical case study of a 68-year-old male, Mr. Jones, presenting with symptoms suggestive of BPH.
Presenting Complaints: Mr. Jones reports increasing frequency and urgency of urination for the past six months. He wakes up two to three times per night to urinate (nocturia). He also describes a weakened urinary stream and a sensation of incomplete bladder emptying. He denies any gross hematuria (blood in urine) or pain. His medical history is significant for hypertension, well-controlled with lisinopril. He is a non-smoker and drinks alcohol occasionally.
Physical Examination: Physical examination reveals a benign abdominal examination. Digital rectal examination (DRE) reveals an enlarged, firm, and slightly nodular prostate. No palpable masses are detected.
Diagnostic Evaluation:
Given Mr. Jones's presentation and physical examination findings, the following diagnostic tests are ordered:
- Urinalysis: To rule out infection and assess for hematuria. A normal urinalysis would support the diagnosis of BPH rather than other urinary tract problems.
- Serum Creatinine and Blood Urea Nitrogen (BUN): To assess renal function, vital for evaluating the safety of potential treatment options. Elevated levels may indicate kidney damage and would require cautious approach to therapy.
- Prostate-Specific Antigen (PSA): Although PSA levels can be elevated in BPH, a significantly elevated PSA raises suspicion of prostate cancer, warranting further investigation like a prostate biopsy. A slightly elevated PSA in the context of BPH is not uncommon.
- Uroflowmetry: To objectively measure the urinary flow rate, providing quantitative data on the severity of urinary obstruction. A decreased flow rate suggests significant obstruction.
- Post-Void Residual (PVR) Measurement: Using ultrasound to assess the amount of urine remaining in the bladder after urination. A high PVR indicates incomplete bladder emptying and potential for urinary retention.
Management Strategies for BPH
The management of BPH is highly individualized, depending on the severity of symptoms and the patient's overall health status. The treatment goals are to relieve symptoms, prevent complications, and maintain quality of life.
Conservative Management:
For men with mild symptoms or who prefer to avoid medication, conservative management strategies may be employed:
- Lifestyle Modifications: Increasing fluid intake (especially water) during the day and decreasing it before bed can help reduce nocturia. Avoiding caffeine and alcohol, particularly before bedtime, can also be beneficial.
- Timed Voiding: Establishing a regular urination schedule can help manage frequency and urgency.
- Pelvic Floor Exercises: Kegel exercises can strengthen the pelvic floor muscles, improving urinary control.
Medical Management:
Medical therapy is often the first-line treatment for moderate to severe symptoms:
- Alpha-blockers: These medications relax the smooth muscles in the prostate and bladder neck, improving urinary flow. Common examples include tamsulosin, terazosin, and alfuzosin. Side effects can include dizziness, hypotension, and retrograde ejaculation.
- 5α-Reductase Inhibitors: These medications decrease the production of DHT, reducing prostate size over time. Finasteride and dutasteride are commonly used. Side effects include decreased libido, erectile dysfunction, and gynecomastia (breast enlargement).
- Combination Therapy: Combining alpha-blockers and 5α-reductase inhibitors can provide greater symptom relief than either medication alone. This approach is often favored for men with significant symptoms.
- Phosphodiesterase-5 Inhibitors: PDE5 inhibitors, like tadalafil, can be used to treat erectile dysfunction, a common side effect of some BPH medications. They should be used cautiously, especially in patients with cardiovascular issues.
Minimally Invasive Therapies:
For men who don't respond to medical therapy or prefer to avoid long-term medication, minimally invasive therapies may be considered:
- Transurethral Microwave Thermotherapy (TUMT): This procedure uses microwave energy to heat and destroy prostate tissue.
- Transurethral Needle Ablation (TUNA): This procedure uses radiofrequency energy to destroy prostate tissue.
- Laser Therapy: Various laser techniques, such as holmium laser enucleation of the prostate (HoLEP) and photoselective vaporization of the prostate (PVP), are used to remove or vaporize prostate tissue.
Surgery:
Surgical intervention is typically reserved for men with severe symptoms, complications like urinary retention, or those who fail to respond to other treatments:
- Transurethral Resection of the Prostate (TURP): This is a widely used surgical procedure to remove excess prostate tissue using a resectoscope.
- Open Prostatectomy: This is a more invasive surgical procedure that involves removing a larger portion of the prostate.
Mr. Jones's Management Plan
Based on Mr. Jones's presentation, diagnostic findings, and preferences, a tailored management plan is developed:
Initially, conservative measures are recommended, including timed voiding, increasing daytime fluid intake, and decreasing evening fluid intake. Given the moderate severity of his symptoms, he is also started on tamsulosin, an alpha-blocker, to improve urinary flow. His symptoms are carefully monitored. If his symptoms don't improve adequately within a few months, the possibility of adding a 5α-reductase inhibitor or considering minimally invasive therapies will be discussed. Regular follow-up appointments are scheduled to monitor his progress and adjust treatment as needed. A discussion regarding the risks and benefits of each treatment option, as well as the potential side effects of medications, is vital in patient education.
Conclusion: Holistic Approach to BPH Management
Effective management of BPH requires a holistic approach that considers not only the patient's physical symptoms but also his overall health, lifestyle, and preferences. A collaborative effort between the patient and healthcare provider is crucial in developing an individualized management plan that maximizes symptom relief, minimizes complications, and improves the patient’s quality of life. Regular monitoring and adjustments to the treatment plan are essential to ensure optimal outcomes. The patient’s understanding and adherence to the treatment plan are equally important for successful management of BPH. This case study underscores the importance of thorough assessment, appropriate diagnostic testing, and a tailored treatment approach in managing this prevalent condition. Further research into the pathophysiology and management of BPH is ongoing, leading to continuous improvements in treatment strategies and better patient outcomes.
Latest Posts
Latest Posts
-
Where Are Most Accenture Clients With Their Generative Ai Journeys
Mar 14, 2025
-
Heart Of Darkness Part 2 Summary
Mar 14, 2025
-
Official Advancement Handbooks Are Available From What Official Source
Mar 14, 2025
-
Knowledge Drill 9 7 Serum Appearance
Mar 14, 2025
-
Unit 8 Worksheet 1 Mole Relationships
Mar 14, 2025
Related Post
Thank you for visiting our website which covers about Hesi Case Study Benign Prostatic Hyperplasia . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
