Hesi Case Study Congenital Heart Disease
Onlines
Apr 06, 2025 · 6 min read
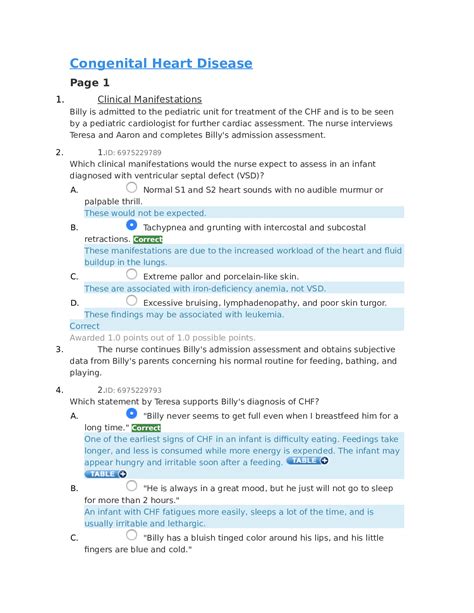
Table of Contents
HESI Case Study: Congenital Heart Disease – A Comprehensive Guide
Congenital heart disease (CHD) encompasses a broad spectrum of structural abnormalities affecting the heart's development before birth. These defects can range from mild to life-threatening, requiring varying levels of medical intervention. Understanding CHD requires a thorough grasp of its diverse presentations, associated complications, and comprehensive management strategies. This article delves into a detailed analysis of HESI case studies focusing on congenital heart defects, providing a framework for understanding the pathophysiology, clinical manifestations, diagnostic approaches, and therapeutic interventions involved.
Understanding the Spectrum of Congenital Heart Defects
Congenital heart defects are classified into cyanotic and acyanotic categories, based on the presence or absence of deoxygenated blood mixing with oxygenated blood. This distinction is crucial in determining the clinical presentation and management approach.
Acyanotic CHDs:
- Ventricular Septal Defect (VSD): A hole in the septum separating the ventricles, allowing blood to shunt from the left ventricle to the right ventricle. This increases pulmonary blood flow, potentially leading to pulmonary hypertension.
- Atrial Septal Defect (ASD): A hole in the septum separating the atria, causing a left-to-right shunt. Similar to VSD, this can lead to increased pulmonary blood flow and potential long-term complications.
- Patent Ductus Arteriosus (PDA): Failure of the ductus arteriosus, a fetal vessel connecting the aorta and pulmonary artery, to close after birth. This results in a left-to-right shunt, increasing pulmonary blood flow.
- Coarctation of the Aorta: Narrowing of the aorta, causing increased pressure in the upper body and decreased blood flow to the lower extremities.
Cyanotic CHDs:
- Tetralogy of Fallot (TOF): A complex defect involving four abnormalities: ventricular septal defect, pulmonary stenosis, overriding aorta, and right ventricular hypertrophy. This leads to mixing of oxygenated and deoxygenated blood, resulting in cyanosis.
- Transposition of the Great Arteries (TGA): The aorta and pulmonary artery are switched, causing deoxygenated blood to circulate through the systemic circulation and oxygenated blood to the lungs.
- Truncus Arteriosus: Failure of the embryonic truncus arteriosus to divide into the aorta and pulmonary artery, resulting in a single great artery receiving blood from both ventricles.
- Tricuspid Atresia: Absence of the tricuspid valve, preventing blood flow from the right atrium to the right ventricle.
Common Clinical Manifestations of CHD
The clinical presentation of CHD is highly variable and depends on the specific defect and its severity. However, some common signs and symptoms include:
- Cyanosis: Bluish discoloration of the skin and mucous membranes due to reduced oxygen saturation in the blood.
- Tachypnea: Rapid breathing, often due to increased pulmonary blood flow or impaired gas exchange.
- Tachycardia: Rapid heart rate, reflecting the body's attempt to compensate for decreased cardiac output.
- Dyspnea: Shortness of breath, reflecting the increased workload on the heart and lungs.
- Fatigue and lethargy: Due to reduced oxygen delivery to the tissues.
- Feeding difficulties: Infants with CHD may tire easily during feeding due to increased cardiac workload.
- Poor weight gain: Poor oxygenation and increased energy expenditure can hinder growth.
- Murmurs: Abnormal heart sounds heard during auscultation, often indicative of turbulent blood flow through the heart.
Diagnostic Approaches to CHD
Accurate diagnosis of CHD involves a comprehensive evaluation using several techniques:
- Physical Examination: Auscultation for murmurs, assessment of pulses, and observation for cyanosis are crucial initial steps.
- Electrocardiogram (ECG): Provides information about the heart's rhythm, conduction system, and chamber size.
- Chest X-ray: Reveals the size and shape of the heart and lungs, providing clues about pulmonary blood flow and cardiac enlargement.
- Echocardiogram: Utilizes ultrasound to visualize the heart's structures and blood flow patterns, providing detailed information about the location and severity of CHD.
- Cardiac Catheterization: A more invasive procedure that allows for direct visualization of the heart chambers and vessels, and provides precise measurements of pressure and blood flow.
Therapeutic Interventions for CHD
Treatment for CHD varies widely depending on the specific defect, its severity, and the patient's overall condition. Interventions may include:
- Medical Management: Medication such as diuretics, digoxin, and ACE inhibitors are used to manage symptoms and improve cardiac function. Prophylactic antibiotics may be prescribed to prevent endocarditis.
- Surgical Interventions: Various surgical techniques are used to repair or palliate CHD. These include:
- Cardiac Surgery: Open-heart surgery to repair structural defects, such as closing VSDs or ASDs, repairing valve abnormalities, or performing arterial switches.
- Catheterization Interventions: Less invasive procedures performed through a catheter, such as balloon atrial septostomy for TGA or balloon valvuloplasty for pulmonary stenosis.
- Palliative Care: When complete surgical correction is not feasible, palliative procedures aim to improve the patient's quality of life and reduce symptoms.
HESI Case Study Examples and Analysis
Let's examine hypothetical HESI case studies to illustrate the application of the principles discussed above.
Case Study 1: A 2-month-old infant presents with cyanosis, tachypnea, and a systolic murmur. Physical examination reveals clubbing of the fingers and toes.
This presentation strongly suggests a cyanotic CHD. Differential diagnoses could include Tetralogy of Fallot, transposition of the great arteries, or tricuspid atresia. Further investigations such as ECG, chest X-ray, and echocardiogram are essential to confirm the diagnosis and determine the specific defect. The clubbing suggests chronic hypoxemia.
Case Study 2: A 6-year-old child is brought to the clinic complaining of fatigue, shortness of breath, and recurrent respiratory infections. Physical examination reveals a loud systolic murmur at the left sternal border.
This presentation is suggestive of an acyanotic CHD, potentially a ventricular septal defect (VSD) or atrial septal defect (ASD). ECG, chest X-ray, and echocardiogram will help delineate the specific diagnosis. The recurrent respiratory infections may be linked to increased pulmonary blood flow.
Case Study 3: An adolescent presents with leg pain and fatigue after strenuous exercise. Blood pressure is significantly higher in the upper extremities than in the lower extremities.
This clinical picture points towards coarctation of the aorta. The difference in blood pressure reflects the narrowed section of the aorta, resulting in reduced blood flow to the lower extremities. Echocardiogram and cardiac catheterization are important diagnostic tools.
Long-Term Management and Considerations
Even after successful surgical repair or medical management, individuals with CHD require lifelong follow-up care. This includes:
- Regular Cardiac Check-ups: To monitor cardiac function, detect any potential complications, and adjust medication as needed.
- Echocardiograms: Periodic echocardiograms are crucial for evaluating the effectiveness of interventions and identifying any structural changes.
- Lifestyle Modifications: Individuals with CHD may need to modify their lifestyle to reduce the strain on their heart, including dietary adjustments, physical activity limitations, and avoiding high-altitude environments.
- Prophylactic Antibiotics: To prevent infective endocarditis, which is a serious complication in individuals with CHD.
- Psychological Support: Living with CHD can pose psychological challenges, and access to emotional support is important.
Conclusion
Congenital heart disease presents a significant challenge in pediatric and adult cardiology. A thorough understanding of the different types of CHD, their clinical presentations, diagnostic approaches, and treatment strategies is crucial for effective management. The HESI case studies provide valuable practice scenarios to apply this knowledge and enhance clinical reasoning skills. Early diagnosis and comprehensive management are essential to improve the long-term outcomes for individuals with CHD. Remember that this article provides general information and should not be considered a substitute for professional medical advice. Always consult with a healthcare professional for any health concerns.
Latest Posts
Latest Posts
-
Within The Relevant Range Of Activity Blank
Apr 08, 2025
-
I Want A Wife Judy Brady Pdf
Apr 08, 2025
-
The Graceful Dancer Moved Across The Stage
Apr 08, 2025
-
Which Of The Following Statements Are True Regarding Political Independents
Apr 08, 2025
-
Electron Configuration Worksheet Pogil Answer Key
Apr 08, 2025
Related Post
Thank you for visiting our website which covers about Hesi Case Study Congenital Heart Disease . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.