Hesi Case Study Heart Failure With Atrial Fibrillation
Onlines
Mar 21, 2025 · 7 min read
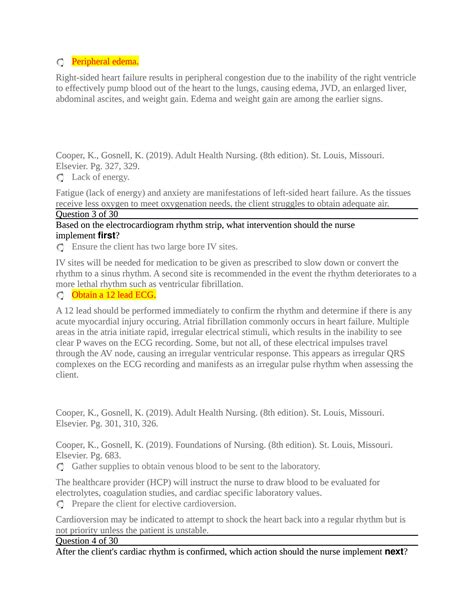
Table of Contents
HESI Case Study: Heart Failure with Atrial Fibrillation – A Comprehensive Analysis
Heart failure (HF) and atrial fibrillation (AFib) are prevalent cardiovascular conditions often co-existing, significantly increasing morbidity and mortality. This article delves into a comprehensive analysis of a hypothetical HESI case study focusing on a patient presenting with heart failure exacerbated by atrial fibrillation. We will explore the pathophysiology, clinical manifestations, diagnostic workup, treatment strategies, and nursing management considerations for this complex clinical scenario.
Understanding the Interplay of Heart Failure and Atrial Fibrillation
Heart failure, a clinical syndrome characterized by the heart's inability to effectively pump blood to meet the body's metabolic demands, presents in various forms, including systolic (reduced ejection fraction) and diastolic (preserved ejection fraction) heart failure. Underlying conditions contributing to HF are numerous and include coronary artery disease (CAD), hypertension, valvular heart disease, and cardiomyopathies.
Atrial fibrillation, the most common sustained cardiac arrhythmia, is characterized by rapid, irregular atrial contractions, leading to disorganized atrial activity and impaired atrial emptying. The consequences of AFib include decreased cardiac output, increased risk of stroke due to thrombus formation in the atria, and potential for heart failure exacerbation.
The interplay between HF and AFib creates a vicious cycle. AFib worsens HF symptoms by reducing cardiac output and increasing myocardial oxygen demand. Conversely, HF can predispose to AFib by increasing atrial stretch and promoting electrical instability. This synergistic relationship makes managing these conditions simultaneously crucial for optimal patient outcomes.
The Hypothetical HESI Case Study: Patient Presentation
Let's consider a hypothetical 72-year-old male patient, Mr. Jones, presenting to the emergency department with complaints of worsening shortness of breath (dyspnea) on exertion, paroxysmal nocturnal dyspnea (PND), and lower extremity edema. He reports a history of hypertension and coronary artery disease, managed with lisinopril and metoprolol. His current symptoms have progressively worsened over the past two weeks. He denies chest pain but admits to experiencing palpitations and feeling generally fatigued.
Vital Signs:
- Blood Pressure: 160/90 mmHg
- Heart Rate: 110 bpm (irregular)
- Respiratory Rate: 24 breaths/min
- Oxygen Saturation: 88% on room air
- Temperature: 98.6°F (37°C)
Physical Examination:
- Cardiovascular: Irregularly irregular rhythm, S3 gallop present, decreased breath sounds at the bases bilaterally, 2+ pitting edema in lower extremities.
- Respiratory: Tachypnea, crackles heard in the lung bases.
- Neurological: Alert and oriented, no focal neurological deficits.
Diagnostic Workup: Unveiling the Clinical Picture
Given Mr. Jones's presentation, a comprehensive diagnostic workup is essential to confirm the diagnoses of HF and AFib and identify any underlying contributing factors. This typically includes:
1. Electrocardiogram (ECG): Confirming Atrial Fibrillation
The ECG is the cornerstone in diagnosing AFib. It will reveal the characteristic absence of P waves, irregularly irregular rhythm, and often a rapid ventricular response. The ECG also helps assess ventricular rate and rhythm, identify any other arrhythmias, and evaluate for signs of ischemia or infarction.
2. Chest X-Ray: Assessing Pulmonary Congestion
A chest X-ray provides valuable information about the presence and extent of pulmonary congestion, a hallmark of heart failure. Findings may include increased cardiothoracic ratio, pleural effusions, and interstitial edema.
3. Echocardiogram: Evaluating Cardiac Function and Structure
An echocardiogram is crucial in assessing left ventricular ejection fraction (LVEF), identifying valvular abnormalities, evaluating left atrial size (which is often enlarged in AFib), and assessing overall cardiac structure and function. This provides essential information for staging heart failure and guiding treatment strategies.
4. Blood Tests: Assessing Renal Function and Markers of Heart Failure
Blood tests are vital in assessing renal function (creatinine, BUN), electrolytes (potassium, sodium), and cardiac biomarkers (BNP, NT-proBNP). Elevated levels of BNP and NT-proBNP are highly indicative of heart failure. Electrolyte imbalances can significantly impact cardiac function and arrhythmias.
5. Other Investigations: Identifying Underlying Causes
Depending on the patient’s history and initial findings, further investigations might be warranted. This could include a coronary angiogram (to assess for CAD), thyroid function tests (to rule out hyperthyroidism), and a Holter monitor (for continuous ECG monitoring to better characterize the AFib).
Management Strategies: A Multifaceted Approach
Managing Mr. Jones's condition necessitates a multi-pronged approach targeting both heart failure and atrial fibrillation:
1. Rate and Rhythm Control: Managing Atrial Fibrillation
Rate control aims to slow the ventricular response to AFib, improving cardiac output and reducing symptoms. This is usually achieved through medications like beta-blockers (metoprolol), calcium channel blockers (diltiazem, verapamil), or digoxin. The choice depends on the patient's comorbidities and tolerance.
Rhythm control aims to restore and maintain sinus rhythm. This can be achieved through medications like antiarrhythmics (amiodarone, flecainide, propafenone) or through cardioversion (electrical or pharmacological). The decision to pursue rhythm control versus rate control depends on several factors, including the patient’s symptoms, LVEF, and the presence of any other comorbidities.
2. Heart Failure Management: Optimizing Cardiac Function
Managing HF involves optimizing cardiac function and reducing symptoms. This includes:
- Diuretics: To reduce fluid overload and pulmonary congestion. Examples include furosemide and bumetanide.
- ACE Inhibitors (ACEi) or Angiotensin Receptor Blockers (ARBs): To reduce afterload and improve cardiac output. Examples include lisinopril, ramipril, valsartan, and losartan.
- Beta-blockers: To reduce heart rate, myocardial oxygen demand, and improve cardiac function.
- Aldosterone receptor antagonists (ARAs): To reduce mortality and morbidity in patients with heart failure and reduced ejection fraction. Examples include spironolactone and eplerenone.
- Hydralazine/Isosorbide dinitrate: In select patients with persistent heart failure symptoms despite guideline-directed medical therapy.
3. Anticoagulation: Preventing Thromboembolic Events
Anticoagulation is crucial in preventing stroke, a significant risk associated with AFib. The choice of anticoagulant depends on several factors, including the patient's CHADS2 or CHA2DS2-VASc score (assessing stroke risk), renal function, and bleeding risk. Options include warfarin, direct thrombin inhibitors (dabigatran), factor Xa inhibitors (rivaroxaban, apixaban), or direct thrombin inhibitors.
4. Lifestyle Modifications: Promoting Heart Health
Lifestyle modifications play a vital role in managing HF and AFib. These include:
- Dietary changes: A low-sodium diet is crucial to reduce fluid retention. Limiting alcohol and caffeine intake is also important.
- Regular exercise: Appropriate exercise programs, under medical supervision, can improve cardiovascular fitness.
- Weight management: Achieving and maintaining a healthy weight reduces stress on the heart.
- Smoking cessation: Smoking significantly worsens cardiovascular disease.
- Stress reduction techniques: Stress can exacerbate heart failure symptoms; stress management techniques are beneficial.
Nursing Management: Comprehensive Care for Optimal Outcomes
Nursing management of Mr. Jones requires a holistic approach focusing on:
- Assessment: Continuous monitoring of vital signs, cardiac rhythm, respiratory status, and fluid balance is crucial. Regular assessment of symptoms (dyspnea, edema, fatigue) and medication effectiveness is essential.
- Medication Administration: Accurate and timely administration of medications is paramount. Monitoring for adverse effects is crucial.
- Fluid Balance Monitoring: Careful monitoring of intake and output is essential to manage fluid balance and prevent fluid overload.
- Oxygen Therapy: Supplemental oxygen is often necessary to improve oxygen saturation.
- Patient Education: Providing comprehensive education to the patient and family about the disease process, medication regimen, and lifestyle modifications is essential for successful management and adherence.
- Emotional Support: Patients with HF and AFib often experience anxiety and depression. Providing emotional support and referral to appropriate resources is important.
- Fall Prevention: Patients with HF and AFib are at increased risk of falls due to orthostatic hypotension and medication side effects. Implementing fall prevention strategies is crucial.
- Discharge Planning: Collaborating with the healthcare team to develop a comprehensive discharge plan including medication reconciliation, follow-up appointments, and resources for home healthcare is vital for optimal patient outcomes.
Conclusion: A Collaborative Approach to Effective Management
Managing heart failure with atrial fibrillation requires a collaborative approach involving physicians, nurses, and other healthcare professionals. A comprehensive assessment, appropriate diagnostic testing, and a tailored treatment plan are essential for optimal patient outcomes. By understanding the pathophysiology, clinical manifestations, and management strategies for this complex clinical scenario, healthcare providers can effectively improve the quality of life and prognosis for patients with HF and AFib. Continuous monitoring, patient education, and adherence to the treatment plan are crucial for successful management and prevention of complications. This detailed analysis of a hypothetical HESI case study underscores the importance of holistic and individualized care in managing this challenging patient population. Remember that this information is for educational purposes and should not be considered medical advice. Always consult with a healthcare professional for any health concerns.
Latest Posts
Latest Posts
-
Amoeba Sisters Video Recap Classification Answer Sheet
Mar 27, 2025
-
5 1 Models Of The Atom Answer Key
Mar 27, 2025
-
The Wretched And The Beautiful Pdf
Mar 27, 2025
-
4 07 Putting Your Work Out There
Mar 27, 2025
-
La Doctora Salazar Me Recomienda Un De Pies A Cabeza
Mar 27, 2025
Related Post
Thank you for visiting our website which covers about Hesi Case Study Heart Failure With Atrial Fibrillation . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
