Hesi Case Study On Gestational Diabetes
Onlines
Mar 20, 2025 · 7 min read
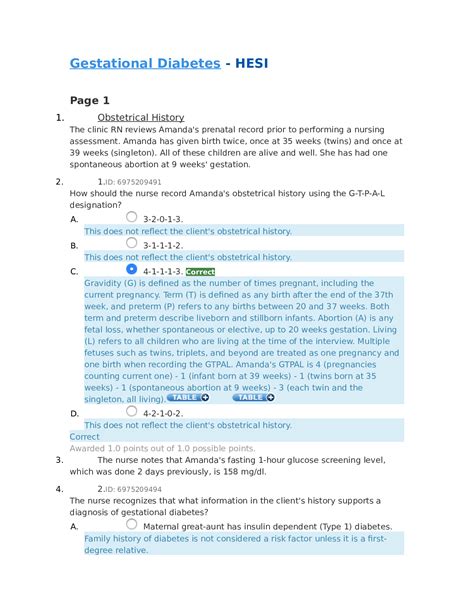
Table of Contents
HESI Case Study: Navigating the Complexities of Gestational Diabetes
Gestational diabetes mellitus (GDM) is a prevalent condition affecting pregnant individuals, posing significant challenges for both the mother and the developing fetus. This comprehensive article delves into a hypothetical HESI case study focusing on a patient diagnosed with GDM, exploring the multifaceted aspects of diagnosis, management, and potential complications. We will examine the crucial role of nursing assessment, intervention, and patient education in achieving optimal outcomes.
The Case: Sarah Miller, 32 Weeks Pregnant
Sarah Miller, a 28-year-old, Caucasian woman, is currently 32 weeks pregnant with her first child. She presents to the clinic for a routine prenatal visit. Her medical history is significant for a family history of type 2 diabetes mellitus (her mother was diagnosed at age 45). Sarah reports gaining 25 pounds during her pregnancy, exceeding the recommended weight gain guidelines. She also complains of increased thirst and frequent urination, particularly at night (polyuria and polydipsia). Her fasting blood glucose level obtained at this visit is 105 mg/dL (high).
Initial Assessment and Diagnostic Testing
Nursing Assessment: The initial nursing assessment is critical in identifying risk factors and potential complications. Key aspects of the assessment include:
- Subjective Data: Detailed history encompassing medical history, family history, current symptoms (polydipsia, polyuria, polyphagia – increased hunger, blurred vision), dietary habits, and lifestyle choices (exercise levels, smoking, alcohol consumption). Gathering information about her understanding of GDM and her pregnancy experience.
- Objective Data: Vital signs, weight, height, BMI calculation, physical examination focusing on skin turgor (assessing for dehydration), assessing for signs of ketoacidosis (fruity breath, deep rapid respirations). Urine analysis for ketones and glucose. Reviewing previous lab results, including blood pressure, and assessing fetal well-being.
Diagnostic Tests: Based on the initial assessment, several diagnostic tests are crucial to confirm the diagnosis of GDM:
- One-step or two-step glucose tolerance test (OGTT or 2-step GTT): This is the gold standard for diagnosing GDM. It involves measuring blood glucose levels after a fasting period and again after consuming a glucose solution. Elevated levels indicate GDM.
- Fasting blood glucose: While a single fasting blood glucose level may not be enough to diagnose GDM, it's a valuable screening tool. An elevated level warrants further testing.
- Glycosylated hemoglobin (HbA1c): This test reflects average blood glucose levels over the past 2-3 months. While not typically used for GDM diagnosis during pregnancy, it can provide valuable information regarding overall glucose control.
Interpretation of Findings
Sarah's fasting blood glucose of 105 mg/dL, coupled with her symptoms and risk factors, necessitates further evaluation with a glucose tolerance test. A positive OGTT would confirm the diagnosis of GDM.
Managing Gestational Diabetes
Management of GDM aims to maintain euglycemia (normal blood glucose levels) throughout the pregnancy to minimize risks to both the mother and the fetus. This involves a multifaceted approach:
1. Dietary Modifications
Dietary changes are the cornerstone of GDM management. Recommendations often include:
- Carbohydrate Counting: Learning to count carbohydrates is essential for regulating blood glucose levels. This allows for appropriate portioning and timing of carbohydrate intake.
- Consistent Meal Timing: Eating at regular intervals prevents blood glucose fluctuations.
- Increased Fiber Intake: High-fiber foods improve glucose tolerance and help regulate blood sugar. Examples include fruits, vegetables, and whole grains.
- Limiting Sugary Drinks: Avoiding sugary beverages like soda and juice is crucial.
- Healthy Fat Intake: Incorporating healthy fats from sources like avocados, nuts, and olive oil.
- Portion Control: Maintaining appropriate portion sizes prevents overconsumption of carbohydrates.
2. Exercise
Regular physical activity plays a vital role in improving insulin sensitivity and glucose control. However, it's essential to choose appropriate exercises and consult with healthcare providers to avoid excessive exertion. Recommended activities include brisk walking, swimming, or cycling for at least 30 minutes on most days of the week.
3. Blood Glucose Monitoring
Regular self-monitoring of blood glucose (SMBG) is critical for managing GDM. This empowers the pregnant person to understand their response to different foods and activities, allowing for timely adjustments to dietary plans or medication. Frequency of SMBG will be determined by the healthcare provider, often involving multiple daily checks.
4. Medication
In some cases, despite dietary modifications and exercise, blood glucose levels may remain uncontrolled. In such situations, medication may be necessary to achieve target glucose ranges.
- Insulin Therapy: Insulin is the most common medication used to manage GDM. Various insulin regimens are available, including basal insulin and mealtime insulin, tailored to individual needs. Insulin does not cross the placenta and is generally safe for the fetus.
- Oral Medications: Oral hypoglycemic agents are generally avoided during pregnancy, except for certain situations in consultation with a specialist.
5. Fetal Surveillance
Regular monitoring of fetal well-being is paramount to ensure a healthy pregnancy outcome. This includes:
- Ultrasound Scans: Ultrasound scans are used to assess fetal growth and development, detecting potential complications like macrosomia (large baby).
- Non-stress Tests (NSTs) and Biophysical Profiles (BPPs): These tests evaluate fetal heart rate patterns and other indicators of fetal well-being.
Potential Complications of GDM
Untreated or poorly managed GDM can lead to various complications for both the mother and the baby:
Maternal Complications:
- Preeclampsia: A condition characterized by high blood pressure and protein in the urine.
- Ketoacidosis: A dangerous condition characterized by excessive ketone production, leading to metabolic acidosis.
- Cesarean Section: Increased risk of requiring a Cesarean section due to macrosomia or other complications.
- Postpartum Hemorrhage: Increased risk of postpartum hemorrhage (heavy bleeding after delivery).
- Increased risk of developing type 2 diabetes later in life.
Fetal/Neonatal Complications:
- Macrosomia: The baby may be excessively large, increasing the risk of birth trauma.
- Hypoglycemia: The baby may experience low blood sugar after birth due to elevated insulin levels in utero.
- Respiratory Distress Syndrome: The baby may experience respiratory difficulties due to immature lung development.
- Hyperbilirubinemia: The baby may have elevated bilirubin levels (jaundice).
- Increased risk of childhood obesity and type 2 diabetes later in life.
Nursing Interventions and Patient Education
The nurse plays a crucial role in providing comprehensive care to pregnant individuals with GDM. Key nursing interventions include:
- Patient Education: Thorough education about GDM, its management, and potential complications is crucial. This includes instructions on dietary modifications, exercise, blood glucose monitoring, and medication administration (if applicable).
- Emotional Support: Providing emotional support to address the stress and anxiety associated with GDM is essential. The patient may benefit from support groups or counseling.
- Monitoring and Assessment: Close monitoring of blood glucose levels, weight, blood pressure, and fetal well-being is essential. Early detection of any complications allows for timely intervention.
- Collaboration with the Healthcare Team: Effective collaboration with other healthcare professionals, including physicians, dietitians, and diabetes educators, ensures comprehensive and coordinated care.
Sarah's Case: Continued Management and Outcomes
Following the diagnosis of GDM, Sarah is educated about dietary management, exercise, and blood glucose monitoring. She is provided with a personalized meal plan and encouraged to attend diabetes education classes. Regular follow-up visits are scheduled to monitor her blood glucose levels and fetal well-being. Despite initial challenges, Sarah diligently follows her treatment plan, showing good compliance. Her blood glucose levels remain well-controlled.
At 37 weeks gestation, she delivers a healthy baby girl via vaginal delivery. The baby's weight is within the normal range, and she experiences no immediate neonatal complications. Postpartum, Sarah's blood glucose levels normalize, and she is counseled on the importance of continued monitoring and lifestyle modifications to reduce her risk of developing type 2 diabetes in the future.
Conclusion
Gestational diabetes is a complex condition requiring comprehensive management to ensure optimal outcomes for both the mother and the baby. The nursing role is multifaceted, involving meticulous assessment, patient education, intervention, and close collaboration with other healthcare providers. By emphasizing early diagnosis, careful monitoring, and appropriate intervention, nurses contribute significantly to improving the health of pregnant individuals with GDM and reducing the risk of long-term complications. This case study highlights the importance of individualized care, empowering the pregnant individual to actively participate in managing her condition and achieving a healthy pregnancy journey. This detailed understanding, incorporating both theoretical knowledge and practical application, is crucial for nursing students preparing for high-stakes examinations like the HESI. The successful management of Sarah's GDM reinforces the importance of proactive care and the positive impact of patient adherence to the treatment plan. This highlights the significance of thorough nursing assessment, effective patient education, and collaborative healthcare in achieving positive pregnancy outcomes for individuals diagnosed with GDM.
Latest Posts
Latest Posts
-
Things Fall Apart Chapter 12 Summary
Mar 20, 2025
-
Lord Of Flies Chapter 8 Summary
Mar 20, 2025
-
Which Of The Following Contains Multiple Gymnosperm Ovules
Mar 20, 2025
-
Letrs Unit 4 Session 2 Check For Understanding
Mar 20, 2025
-
Fundamentals Of Logic Design 7th Edition Solutions
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about Hesi Case Study On Gestational Diabetes . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
