Hesi Chronic Kidney Disease Case Study
Onlines
Mar 18, 2025 · 7 min read
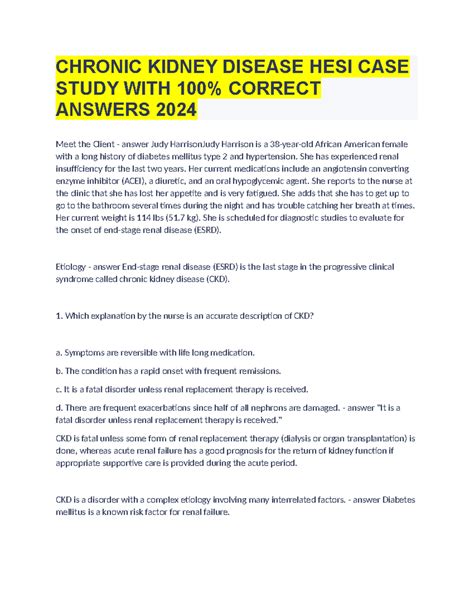
Table of Contents
HESI Chronic Kidney Disease Case Study: A Comprehensive Analysis
Chronic Kidney Disease (CKD) is a significant public health concern, characterized by a gradual loss of kidney function over time. Understanding its multifaceted nature is crucial for healthcare professionals. This in-depth analysis delves into a hypothetical HESI-style case study on CKD, examining its presentation, diagnosis, management, and potential complications. We will explore various aspects of patient care, focusing on evidence-based practices and critical thinking skills essential for effective nursing intervention.
The Case Study: Presenting Symptoms and Initial Assessment
Mr. Jones, a 68-year-old male with a history of type 2 diabetes mellitus and hypertension, presents to the clinic complaining of increasing fatigue, shortness of breath, and swelling in his ankles and feet for the past three months. He reports decreased urine output and reports feeling generally unwell. He denies any chest pain, nausea, or vomiting. His medical history also includes hyperlipidemia, managed with atorvastatin. He is a smoker (one pack per day for 40 years) and admits to a sedentary lifestyle.
Physical Examination: On examination, Mr. Jones appears pale and fatigued. His blood pressure is 160/90 mmHg, heart rate is 88 bpm, and respirations are 22 breaths per minute. Edema is noted in his lower extremities (2+ pitting edema). Auscultation of the lungs reveals crackles bilaterally. Cardiac examination reveals a regular rate and rhythm with no murmurs, rubs, or gallops.
Laboratory Findings: Initial blood work reveals the following:
- Elevated serum creatinine: 3.5 mg/dL (indicative of reduced glomerular filtration rate (GFR))
- Elevated blood urea nitrogen (BUN): 60 mg/dL (further suggesting impaired kidney function)
- Decreased hemoglobin: 9.5 g/dL (suggestive of anemia, a common complication of CKD)
- Elevated potassium: 5.8 mEq/L (hyperkalemia, a potentially life-threatening electrolyte imbalance)
- Metabolic acidosis: Low bicarbonate levels
- Urine analysis: Proteinuria (protein in the urine), indicative of kidney damage
Diagnostic Evaluation and Staging of CKD
Based on Mr. Jones's symptoms, physical examination findings, and laboratory results, CKD is strongly suspected. Further diagnostic tests are necessary to confirm the diagnosis, determine the stage of CKD, and identify the underlying cause. These tests may include:
1. Glomerular Filtration Rate (GFR) Calculation:
The GFR is the best measure of kidney function. The estimated GFR (eGFR) is calculated using the patient's serum creatinine level, age, sex, and race. A reduced eGFR confirms the presence of CKD and helps to stage the disease. Mr. Jones's eGFR is likely significantly below 60 mL/min/1.73 m², placing him in at least stage 3 CKD.
2. Kidney Ultrasound:
This imaging study helps to visualize the kidneys, assess their size and structure, and identify any abnormalities such as cysts, tumors, or obstructions. It can help to rule out other causes of kidney dysfunction.
3. Kidney Biopsy (if indicated):
A kidney biopsy may be performed in certain cases to determine the underlying cause of CKD, particularly if the cause is unclear or if there is suspicion of specific glomerular diseases. This is an invasive procedure and is usually reserved for cases where the information is essential for guiding treatment decisions.
Management and Treatment Strategies
The management of CKD is multifaceted and involves a combination of pharmacological and non-pharmacological interventions. The goals of treatment are to slow the progression of kidney disease, manage symptoms, prevent complications, and improve the patient's quality of life.
1. Blood Pressure Control:
Strict blood pressure control is crucial in slowing the progression of CKD. The goal is usually to achieve a blood pressure below 140/90 mmHg, or even lower in some cases. This often requires the use of multiple antihypertensive medications, such as ACE inhibitors or ARBs, which are particularly beneficial in protecting the kidneys. Mr. Jones's current blood pressure of 160/90 mmHg requires immediate attention and aggressive management.
2. Glycemic Control:
In patients with diabetes, meticulous control of blood glucose levels is essential. This involves optimizing insulin therapy or oral hypoglycemic agents to maintain near-normal blood sugar levels. Tight glycemic control significantly reduces the risk of further kidney damage. Mr. Jones's diabetes management needs a thorough review and potentially adjustment.
3. Dietary Modifications:
Dietary changes are vital for managing CKD. This often includes restricting protein intake, limiting sodium and potassium intake, and controlling fluid intake. A registered dietitian specializing in renal diets can create a personalized plan to meet the patient's nutritional needs while managing electrolyte and fluid balance. For Mr. Jones, this is crucial given his hyperkalemia.
4. Anemia Management:
Anemia is a common complication of CKD. Treatment typically involves erythropoiesis-stimulating agents (ESAs) or iron supplementation. ESAs stimulate red blood cell production, while iron is essential for hemoglobin synthesis. Mr. Jones's low hemoglobin level necessitates appropriate intervention.
5. Management of Hyperkalemia:
Hyperkalemia is a potentially life-threatening electrolyte imbalance. Management may include restricting dietary potassium, using potassium-binding resins (e.g., sodium polystyrene sulfonate), and administering intravenous calcium gluconate in emergencies. Given Mr. Jones's dangerously high potassium level, immediate action is crucial.
6. Phosphate Binder:
Elevated phosphate levels are common in CKD. Phosphate binders, taken with meals, help to bind phosphate in the gut, reducing phosphate absorption.
7. Acid-Base Balance Correction:
Metabolic acidosis is another complication of CKD. Treatment may involve sodium bicarbonate supplementation to correct the acidosis.
8. Lifestyle Modifications:
Lifestyle changes, including smoking cessation, regular exercise, and weight management, are important for overall health and can help slow the progression of CKD. These are vital for Mr. Jones's overall well-being and should be strongly emphasized.
Potential Complications and Long-Term Management
CKD significantly increases the risk of various complications, including cardiovascular disease, infections, bone disease, and ultimately, end-stage renal disease (ESRD). Careful monitoring and proactive management of these potential complications are critical.
-
Cardiovascular Disease: CKD patients are at a significantly increased risk of cardiovascular events, including heart attacks and strokes. This risk is driven by several factors, including hypertension, hyperlipidemia, anemia, and inflammation. Aggressive management of cardiovascular risk factors is crucial.
-
Infections: Impaired immune function increases susceptibility to infections in CKD patients. Careful monitoring for signs and symptoms of infection, along with prompt treatment, is essential.
-
Bone Disease: CKD can lead to secondary hyperparathyroidism and bone disease. This may require treatment with vitamin D analogs and phosphate binders.
-
End-Stage Renal Disease (ESRD): In advanced CKD, kidney function may deteriorate to the point that dialysis or kidney transplantation becomes necessary. Discussions about these options should begin early in the course of the disease to allow the patient adequate time to make informed decisions.
Nursing Interventions and Patient Education
Nursing care for patients with CKD focuses on providing comprehensive assessment, education, and support.
-
Assessment: Regular monitoring of vital signs, weight, urine output, and electrolyte levels is essential. Assessment of the patient's overall health status, including nutritional status and symptom management, is also crucial.
-
Education: Patient and family education is vital for successful self-management of CKD. Education should cover dietary restrictions, medication management, symptom management, and potential complications.
-
Support: Providing emotional and psychological support is essential, as CKD can significantly impact a patient's quality of life. Referral to support groups or counseling services may be beneficial.
Conclusion
This detailed case study demonstrates the complexity of managing CKD. Early diagnosis, aggressive management of risk factors, and meticulous attention to detail are essential for slowing disease progression, preventing complications, and improving the patient's quality of life. Multidisciplinary teamwork, involving nephrologists, dietitians, nurses, and other healthcare professionals, is crucial for providing optimal care for patients with CKD. The focus on evidence-based practice, alongside empathetic patient care, forms the cornerstone of successful CKD management. Mr. Jones's case highlights the need for proactive intervention and patient education in order to achieve the best possible outcomes. Continuous monitoring and reassessment are vital in managing the dynamic nature of this chronic condition.
Latest Posts
Latest Posts
-
The Spirit Catches You And You Fall Down Quotes
Mar 19, 2025
-
Alabanzas Ala Virgen De Guadalupe Letra
Mar 19, 2025
-
Work Energy Theorem Color By Number
Mar 19, 2025
-
A Raisin In The Sun Major Works Data Sheet
Mar 19, 2025
-
Hardware Lab Simulation 9 1 Syncing To The Cloud
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about Hesi Chronic Kidney Disease Case Study . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
