Hypoxemia Can Be Evidenced On Physical Exam As
Onlines
Mar 28, 2025 · 6 min read
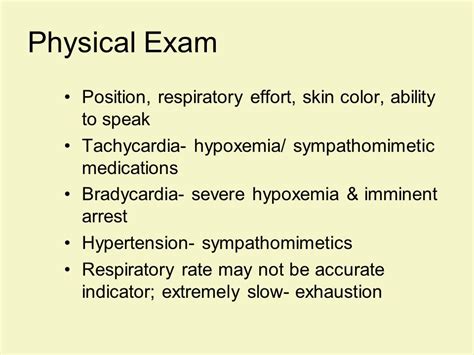
Table of Contents
Hypoxemia: Physical Exam Findings and Clinical Significance
Hypoxemia, a condition characterized by abnormally low levels of oxygen in the blood, is a serious medical issue that can manifest through a variety of physical exam findings. While arterial blood gas (ABG) analysis is the gold standard for diagnosing hypoxemia, astute observation during the physical exam can provide crucial clues, guiding further investigations and prompting timely interventions. This article will delve into the physical examination signs associated with hypoxemia, emphasizing the importance of a thorough and systematic approach.
Recognizing the Manifestations of Hypoxemia: A Comprehensive Guide
Hypoxemia's clinical presentation is highly variable, depending on the severity, underlying cause, and individual patient factors. However, some common physical exam findings consistently point towards this life-threatening condition. It is important to remember that these signs are not specific to hypoxemia and can be seen in other conditions, emphasizing the importance of considering the patient's complete clinical picture.
Respiratory System:
-
Tachypnea: Increased respiratory rate is a hallmark sign of hypoxemia. The body attempts to compensate for low oxygen levels by increasing ventilation to take in more oxygen. Observe the respiratory rate, noting any significant deviations from the normal range. Tachypnea, often accompanied by dyspnea (shortness of breath), is a key indicator that requires immediate attention.
-
Dyspnea: Difficulty breathing, ranging from mild breathlessness to severe air hunger, is a common symptom. Assess the patient's level of dyspnea using a standardized scale, noting their ability to speak in full sentences, their posture (e.g., tripod positioning), and any use of accessory muscles. Severe dyspnea warrants prompt oxygen supplementation and further investigation.
-
Use of Accessory Muscles: In severe hypoxemia, patients may recruit accessory muscles – like the sternocleidomastoid, scalene, and intercostal muscles – to aid in breathing. Observe for the use of these muscles, as it signifies increased respiratory effort and potential respiratory distress.
-
Cyanosis: A bluish discoloration of the skin and mucous membranes is a late sign of hypoxemia. While cyanosis can be a visible indicator, it's not always reliable, as it can be masked by anemia or other factors. Focus on checking the mucous membranes (e.g., lips, tongue, nail beds) for cyanosis as they provide more accurate assessment.
-
Abnormal Breath Sounds: Auscultation of the lungs using a stethoscope can reveal abnormal breath sounds indicative of underlying respiratory pathology contributing to hypoxemia. These could include wheezes (indicative of airway narrowing), crackles (indicative of fluid in the lungs), or diminished breath sounds (indicative of air trapping or lung consolidation). Thorough lung auscultation is crucial in differentiating the cause of hypoxemia.
-
Cough: A productive or non-productive cough may accompany hypoxemia, particularly if it's due to underlying respiratory infections, aspiration, or pulmonary edema. Note the character of the cough (e.g., dry, wet, productive), the sputum's characteristics (if present), and its frequency.
Cardiovascular System:
-
Tachycardia: Increased heart rate is a common compensatory response to hypoxemia. The heart attempts to increase oxygen delivery to tissues by pumping faster. Observe the heart rate, noting any significant increase from the patient's baseline.
-
Hypotension: In severe hypoxemia, decreased oxygen delivery can lead to decreased cardiac output and hypotension (low blood pressure). Monitor blood pressure to assess for this complication. Hypotension indicates a serious deterioration and needs immediate management.
-
Arrhythmias: Hypoxemia can disrupt the heart's electrical conduction system, potentially leading to arrhythmias like tachycardia, bradycardia, or atrial fibrillation. Continuous cardiac monitoring is essential in patients with suspected hypoxemia, particularly those with pre-existing cardiac conditions.
Neurological System:
-
Altered Mental Status: Hypoxemia can affect brain function, leading to changes in mental status such as confusion, disorientation, lethargy, or even coma. Assess the patient's level of consciousness using the Glasgow Coma Scale or similar tools. Altered mental status is a critical finding that needs prompt attention.
-
Headache: Headache can be an early symptom of hypoxemia. This is because a lack of oxygen can cause vasodilation in the brain, which stimulates pain receptors. Inquire about the onset, nature, and severity of any headache.
-
Restlessness or Anxiety: As the brain becomes oxygen-deprived, patients may exhibit restlessness, anxiety, or irritability. These behavioral changes can be subtle early signs of hypoxemia.
Other Systems:
-
Clubbing: While not directly caused by hypoxemia, clubbing (widening and rounding of the fingertips) can be an indicator of chronic hypoxemia, particularly in conditions like congenital heart disease or chronic lung diseases.
-
Peripheral Cyanosis: Cyanosis in the extremities can be a sign of reduced peripheral blood flow, which may be seen in hypoxemic patients.
Differential Diagnosis and Further Investigations
The physical examination findings associated with hypoxemia are not specific. Many other conditions can mimic the symptoms. Therefore, a thorough history and physical examination, including vital signs monitoring and appropriate diagnostic tests, are crucial to determine the underlying cause and guide management. Differential diagnoses may include pneumonia, pulmonary embolism, asthma, COPD, heart failure, and carbon monoxide poisoning.
Further investigations may include:
-
Arterial Blood Gas (ABG) analysis: This is the gold standard for diagnosing hypoxemia, measuring the partial pressure of oxygen (PaO2) and oxygen saturation (SaO2).
-
Pulse oximetry: A non-invasive method to measure oxygen saturation (SpO2), providing a quick assessment of oxygenation. However, it’s important to note that pulse oximetry readings might not always be accurate in certain situations (e.g., poor peripheral perfusion, presence of certain pigments).
-
Chest X-ray: To identify underlying lung pathologies such as pneumonia, pneumothorax, or pulmonary edema.
-
Electrocardiogram (ECG): To assess for cardiac arrhythmias.
-
Echocardiogram: To evaluate cardiac function.
-
Computed Tomography (CT) scan: To assess for pulmonary embolism or other abnormalities.
Management of Hypoxemia
The management of hypoxemia depends on the underlying cause and severity. Supplemental oxygen therapy is often the initial treatment, delivered via nasal cannula, face mask, or high-flow oxygen devices, depending on the patient's needs. For severe hypoxemia, mechanical ventilation may be required. Treatment of the underlying cause is crucial to resolve the hypoxemia and prevent recurrence. This may involve antibiotics for pneumonia, anticoagulants for pulmonary embolism, bronchodilators for asthma or COPD, and other appropriate treatments.
Conclusion
Hypoxemia is a serious medical condition requiring prompt diagnosis and management. While ABG analysis is the definitive diagnostic tool, a careful physical examination plays a crucial role in identifying potential cases of hypoxemia. Recognizing the subtle and overt signs and symptoms discussed above will help healthcare professionals initiate timely investigations and appropriate management, improving patient outcomes. Remember to always consider the patient's overall clinical picture, correlating physical findings with vital signs, medical history, and the results of appropriate investigations to reach a comprehensive diagnosis and effective treatment plan. The ability to recognize the early signs of hypoxemia is a crucial skill for any healthcare professional, potentially saving lives through prompt intervention.
Latest Posts
Latest Posts
-
7 15 Unit Test Social And Sexual Health Part 1
Mar 31, 2025
-
Most Dangerous Ways To School Bolivia Worksheet Answers
Mar 31, 2025
-
Choose The Statement Below That Explains What Closing Means
Mar 31, 2025
-
Activity 2 3 1 Hexadecimal And Octal Number Systems
Mar 31, 2025
-
3 04 Quiz Poetry Of The Harlem Renaissance
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about Hypoxemia Can Be Evidenced On Physical Exam As . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
