Match Each Antibacterial Medication With Its Appropriate Mechanism Of Action.
Onlines
Mar 14, 2025 · 5 min read
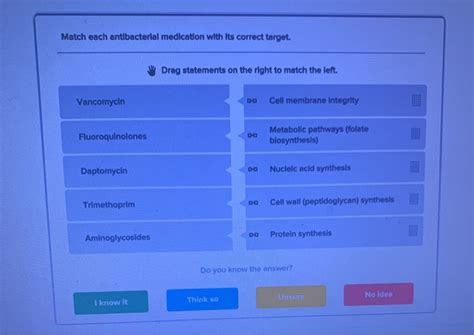
Table of Contents
Matching Antibacterial Medications with Their Mechanisms of Action
Antibacterial medications, also known as antibiotics, are a cornerstone of modern medicine, combating bacterial infections that range from minor skin infections to life-threatening sepsis. However, understanding how these medications work is crucial for effective treatment and combating the growing threat of antibiotic resistance. This comprehensive guide will delve into the mechanisms of action of various antibacterial medications, categorizing them for clarity and providing illustrative examples.
Major Mechanisms of Action: A Categorical Overview
Antibacterial medications achieve their antimicrobial effects through various mechanisms, primarily targeting essential bacterial processes. These mechanisms can be broadly categorized as follows:
1. Inhibition of Cell Wall Synthesis
This is arguably the most common mechanism of action. Bacterial cell walls, unlike eukaryotic cells, contain peptidoglycan, a crucial structural component. Medications targeting cell wall synthesis disrupt this structure, leading to bacterial cell lysis (rupture) and death.
-
Beta-lactams: This is a large and diverse group, including penicillins, cephalosporins, carbapenems, and monobactams. They all contain a beta-lactam ring, which inhibits penicillin-binding proteins (PBPs), enzymes responsible for peptidoglycan synthesis. This inhibition prevents cross-linking of peptidoglycan chains, weakening the cell wall.
- Penicillins (e.g., penicillin G, amoxicillin): Effective against Gram-positive bacteria, with varying effectiveness against Gram-negative bacteria.
- Cephalosporins (e.g., cefazolin, ceftriaxone): A broader spectrum than penicillins, with generations exhibiting increasing activity against Gram-negative bacteria.
- Carbapenems (e.g., imipenem, meropenem): Very broad-spectrum antibiotics, effective against many Gram-positive and Gram-negative bacteria, including some resistant strains.
- Monobactams (e.g., aztreonam): Primarily active against Gram-negative aerobic bacteria.
-
Glycopeptides (e.g., vancomycin, teicoplanin): These antibiotics bind to the D-alanyl-D-alanine terminus of peptidoglycan precursors, preventing their incorporation into the growing peptidoglycan chain. They are primarily effective against Gram-positive bacteria, especially those resistant to beta-lactams.
-
Bacitracin: This topical antibiotic inhibits the dephosphorylation of bactoprenol phosphate, a lipid carrier involved in peptidoglycan transport across the cytoplasmic membrane. This prevents the delivery of peptidoglycan precursors to the cell wall.
2. Inhibition of Protein Synthesis
Bacterial protein synthesis is a complex process involving ribosomes, messenger RNA (mRNA), and transfer RNA (tRNA). Several antibiotics target different stages of this process, leading to bacterial death.
-
Aminoglycosides (e.g., gentamicin, tobramycin, amikacin): These antibiotics bind irreversibly to the 30S ribosomal subunit, causing misreading of mRNA and inhibiting protein synthesis. They are effective against many Gram-negative and some Gram-positive bacteria. They are often used synergistically with other antibiotics.
-
Tetracyclines (e.g., tetracycline, doxycycline, minocycline): These antibiotics reversibly bind to the 30S ribosomal subunit, blocking the attachment of aminoacyl-tRNA to the mRNA-ribosome complex. This inhibits protein synthesis and is effective against a broad range of bacteria.
-
Macrolides (e.g., erythromycin, azithromycin, clarithromycin): These antibiotics reversibly bind to the 50S ribosomal subunit, inhibiting translocation (movement of the ribosome along the mRNA). They are effective against many Gram-positive bacteria and some atypical bacteria.
-
Chloramphenicol: This antibiotic binds to the 50S ribosomal subunit, inhibiting peptidyl transferase activity, a crucial step in peptide bond formation. It has a broad spectrum of activity but significant toxicity concerns.
-
Lincosamides (e.g., clindamycin, lincomycin): These antibiotics bind to the 50S ribosomal subunit, preventing peptide bond formation. They are effective against Gram-positive bacteria and some anaerobic bacteria.
-
Oxazolidinones (e.g., linezolid): These antibiotics bind to the 50S ribosomal subunit, inhibiting the initiation of protein synthesis. They are active against Gram-positive bacteria, including those resistant to other antibiotics.
3. Inhibition of Nucleic Acid Synthesis
Bacterial DNA and RNA synthesis are essential for bacterial replication and growth. Several antibiotics target these processes.
-
Quinolones (e.g., ciprofloxacin, levofloxacin, moxifloxacin): These antibiotics inhibit topoisomerases, enzymes essential for DNA replication and repair. They have a broad spectrum of activity, effective against many Gram-positive and Gram-negative bacteria.
-
Rifampin: This antibiotic inhibits bacterial DNA-dependent RNA polymerase, preventing RNA synthesis. It is often used in combination with other antibiotics for the treatment of tuberculosis and other infections.
-
Metronidazole: This antibiotic disrupts DNA synthesis in anaerobic bacteria and protozoa by interfering with DNA structure. It is effective against various anaerobic infections.
4. Inhibition of Metabolic Pathways
Some antibiotics target specific metabolic pathways essential for bacterial survival.
- Sulfonamides (e.g., sulfamethoxazole) and Trimethoprim: These antibiotics are often used in combination (co-trimoxazole). Sulfonamides inhibit dihydropteroate synthase, an enzyme involved in folic acid synthesis, while trimethoprim inhibits dihydrofolate reductase, another enzyme in the same pathway. Folic acid is essential for bacterial DNA synthesis. This combination provides synergistic activity.
Understanding the Spectrum of Activity
Antibacterial medications exhibit varying spectra of activity.
-
Narrow-spectrum antibiotics: Effective against a limited range of bacterial species. For example, penicillin G is primarily effective against Gram-positive bacteria.
-
Broad-spectrum antibiotics: Effective against a wide range of bacterial species, including both Gram-positive and Gram-negative bacteria. Tetracyclines and fluoroquinolones are examples of broad-spectrum antibiotics.
The Ever-Present Threat of Antibiotic Resistance
The widespread use of antibiotics has led to the emergence and spread of antibiotic-resistant bacteria. Bacteria can develop resistance through various mechanisms, including mutations in target enzymes, efflux pumps (expelling the antibiotic), and enzymatic inactivation of the antibiotic. This necessitates careful antibiotic stewardship, including appropriate prescribing practices and the development of new antibacterial agents.
Conclusion: A Complex Landscape of Antibacterial Action
This detailed overview demonstrates the diversity of mechanisms by which antibacterial medications combat bacterial infections. Understanding these mechanisms is critical for clinicians in selecting appropriate antibiotics, optimizing treatment strategies, and mitigating the escalating problem of antibiotic resistance. Continuous research and development of new antibiotics with novel mechanisms of action are crucial to maintaining the effectiveness of antibacterial therapies in the face of evolving bacterial resistance. The information provided here should not be considered a substitute for professional medical advice. Always consult with a healthcare provider for diagnosis and treatment of any bacterial infection.
Latest Posts
Latest Posts
-
At Kairas Caribbean Cuisine Kaira Improves Focuses On Efficiency By
Mar 14, 2025
-
Of Paramount Significance In The Tabernacle Was The
Mar 14, 2025
-
A Properly Written Statement Of Work Will
Mar 14, 2025
-
Identify An Accurate Statement About Ethnocentrism
Mar 14, 2025
-
What Do The Police Put On A Bad Pig
Mar 14, 2025
Related Post
Thank you for visiting our website which covers about Match Each Antibacterial Medication With Its Appropriate Mechanism Of Action. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
