Medical Decision Making Is Based On Which Of The Following
Onlines
Mar 29, 2025 · 6 min read
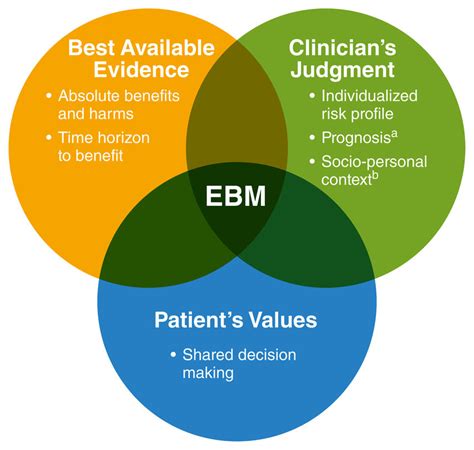
Table of Contents
Medical Decision-Making: A Deep Dive into the Foundational Principles
Medical decision-making is a complex process, far exceeding a simple checklist or algorithm. It's a multifaceted interplay of scientific evidence, patient values, clinical expertise, and ethical considerations. Understanding the foundations of this process is crucial for both healthcare professionals and patients, empowering informed consent and optimal healthcare outcomes. This article will delve into the key pillars supporting medical decisions, exploring their individual strengths and the crucial interplay between them.
The Pillars of Medical Decision-Making
Several crucial elements underpin sound medical decision-making. These aren't independent entities but rather interwoven strands forming a robust and flexible framework. Let's explore each in detail:
1. Best Available Evidence: The Foundation of Scientific Medicine
The cornerstone of modern medical decision-making rests on the best available scientific evidence. This refers to the rigorous collection, analysis, and interpretation of data through research methodologies like randomized controlled trials, cohort studies, and meta-analyses. Evidence-based medicine (EBM) advocates for integrating this research with clinical expertise and patient values to provide optimal care.
-
Types of Evidence: The hierarchy of evidence is crucial in determining the strength of a recommendation. Systematic reviews and meta-analyses of randomized controlled trials (RCTs) generally hold the highest level of evidence, followed by individual RCTs, cohort studies, case-control studies, and finally, expert opinion. The quality of the evidence also plays a vital role; well-designed studies with low risk of bias are given more weight.
-
Challenges in Evidence-Based Practice: While EBM is a cornerstone of modern medicine, challenges exist. Not all medical questions have robust evidence supporting them. Furthermore, translating research findings into practical clinical applications can be complex, requiring clinicians to critically appraise the evidence's relevance to their individual patients. Access to high-quality research can also be a barrier, particularly in resource-limited settings. Finally, the sheer volume of medical literature can be overwhelming, requiring efficient methods of information retrieval and critical appraisal.
-
Keeping Up-to-Date: The medical landscape is constantly evolving, with new research emerging regularly. Healthcare professionals must commit to lifelong learning, actively seeking out and critically evaluating new evidence to ensure their practice remains current and evidence-based. This involves staying updated with reputable medical journals, attending conferences, and engaging in continuous professional development.
2. Clinical Expertise: The Art and Science of Medicine
Clinical expertise is the knowledge, skills, and judgment accumulated by healthcare professionals through years of training, experience, and reflection. It encompasses not only understanding the scientific evidence but also the ability to apply it effectively in the context of individual patients' circumstances. This involves:
-
Pattern Recognition: Experienced clinicians often develop the ability to recognize subtle patterns and deviations from the norm that might not be immediately apparent in the data. This intuitive understanding, honed by experience, can be invaluable in complex cases.
-
Diagnostic Reasoning: Clinical expertise is essential in making accurate diagnoses. This involves integrating various pieces of information – from the patient's history and physical examination to laboratory results and imaging studies – to formulate a differential diagnosis and ultimately arrive at the most likely diagnosis.
-
Treatment Planning: Clinical expertise guides the selection of appropriate treatment strategies, taking into account the patient's individual characteristics, preferences, and comorbidities. It often involves navigating uncertainties and making informed decisions in situations where evidence might be limited or conflicting.
-
Communication and Interpersonal Skills: Effective communication is integral to clinical expertise. Building rapport with patients, actively listening to their concerns, and effectively explaining complex medical information are crucial for shared decision-making and building trust.
3. Patient Values and Preferences: The Cornerstone of Patient-Centered Care
Patient-centered care emphasizes the patient's autonomy and their right to make informed decisions about their own healthcare. This acknowledges that medical decisions shouldn't be solely based on scientific evidence or clinical expertise; they must also align with the patient's values, preferences, and goals. This includes:
-
Understanding Patient Preferences: It’s critical to understand the patient's personal values, beliefs, and preferences regarding treatment options. Some patients might prioritize quality of life over life extension, while others might hold the opposite view. Some might be risk-averse, while others are willing to take greater risks for potential benefits.
-
Shared Decision-Making: Shared decision-making involves a collaborative conversation between the healthcare professional and the patient, where both parties actively participate in exploring treatment options, weighing their benefits and risks, and ultimately arriving at a decision that aligns with the patient's values and goals. This requires open communication, mutual respect, and a shared understanding of the available information.
-
Cultural Considerations: Cultural background and beliefs can significantly influence patient preferences and healthcare decisions. Healthcare professionals must be aware of and sensitive to these cultural factors to provide culturally competent and patient-centered care.
-
Ethical Considerations: Patient autonomy is a fundamental ethical principle in medicine. Healthcare professionals have an ethical obligation to respect patient preferences, even if those preferences differ from what they might consider to be the "best" medical option. However, this respect is not absolute; there are situations where overriding patient preferences might be justifiable, such as in cases of severe mental illness or situations where the patient's actions might pose a risk to others.
4. Ethical Considerations: Navigating Moral Dilemmas
Ethical considerations play a crucial role in medical decision-making, particularly in situations involving uncertainty, conflict, or limited resources. Ethical principles such as autonomy, beneficence, non-maleficence, and justice guide the decision-making process, ensuring that decisions are made in a morally responsible manner.
-
Autonomy: Respecting the patient's right to make their own decisions about their healthcare.
-
Beneficence: Acting in the best interests of the patient.
-
Non-maleficence: Avoiding harm to the patient.
-
Justice: Ensuring fairness and equity in the distribution of healthcare resources.
-
Ethical Dilemmas: Ethical dilemmas often arise in medical practice, requiring careful consideration of competing values and principles. For instance, a decision regarding end-of-life care might involve balancing the patient's autonomy with the desire to provide comfort and alleviate suffering. Resource allocation decisions often involve ethical considerations of justice and fairness.
The Interplay of Factors: A Holistic Approach
It’s crucial to recognize that these four pillars are not independent but rather intertwined and mutually influential. Effective medical decision-making necessitates a holistic approach that considers all aspects:
-
Evidence informs clinical expertise, but expertise guides the interpretation and application of evidence. Experienced clinicians can recognize nuances and exceptions to general rules based on their understanding of individual patients.
-
Patient values shape the application of both evidence and expertise. The "best" evidence-based treatment might not be the most suitable option for a particular patient if it conflicts with their values or preferences.
-
Ethical considerations influence all aspects of the decision-making process, ensuring that decisions are made in a responsible and morally sound manner. Ethical reflection is essential when navigating conflicts between evidence, expertise, and patient values.
Conclusion: Towards Informed and Ethical Healthcare
Medical decision-making is a complex, dynamic process requiring a nuanced understanding of scientific evidence, clinical expertise, patient values, and ethical considerations. By integrating these four pillars, healthcare professionals can strive toward informed, patient-centered, and ethically sound decisions that ultimately contribute to improved healthcare outcomes. Continuous learning, critical appraisal of evidence, effective communication, and a commitment to ethical principles are essential for navigating the challenges and complexities inherent in this crucial aspect of medical practice. The future of medicine hinges on this holistic, collaborative, and patient-focused approach to decision-making. This approach ensures not only better health outcomes but also strengthens the vital doctor-patient relationship built on trust, understanding, and shared responsibility.
Latest Posts
Latest Posts
-
Which Of The Following Is An Example Of Green Computing
Mar 31, 2025
-
Summary For Chapter 11 To Kill A Mockingbird
Mar 31, 2025
-
Which Drive Is Displayed First In The Command Window
Mar 31, 2025
-
Which Of The Following Diagrams Involves A Virtual Image
Mar 31, 2025
-
Which Of The Following Statements About Gerrymandering Is True
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about Medical Decision Making Is Based On Which Of The Following . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
