Neuromuscular Disorders Impair Lung Function Primarily Because Of
Onlines
Mar 04, 2025 · 6 min read
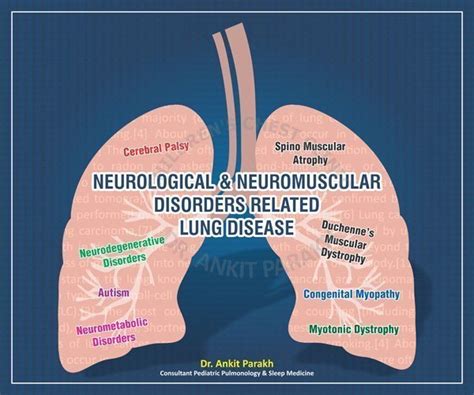
Table of Contents
Neuromuscular Disorders Impair Lung Function Primarily Because of…
Neuromuscular disorders (NMDs) encompass a diverse group of diseases affecting the nerves, muscles, or the neuromuscular junction, the point where nerve and muscle meet. While the primary manifestation of these disorders is often muscle weakness or atrophy, a significant and often overlooked consequence is impaired lung function. This impairment is not a secondary effect, but a direct and crucial factor influencing the quality of life and prognosis for individuals with NMDs. This article will delve into the multifaceted ways in which NMDs impair lung function, exploring the underlying mechanisms and their clinical implications.
The Mechanics of Respiratory Muscle Weakness
The most fundamental reason why NMDs impair lung function is respiratory muscle weakness. Breathing isn't merely a passive process; it relies on the coordinated action of several powerful muscles, including the diaphragm, intercostal muscles, and accessory muscles like the sternocleidomastoids and scalenes. These muscles contract rhythmically, expanding the chest cavity and drawing air into the lungs (inspiration), and then relaxing to allow the lungs to recoil and expel air (expiration). In NMDs, the nerves that innervate these muscles are damaged, leading to progressive muscle weakness and atrophy.
Diaphragmatic Dysfunction: The Central Player
The diaphragm, a sheet of muscle separating the chest and abdomen, is the primary muscle of inspiration. Its dysfunction has profound consequences on lung function. Weakening of the diaphragm reduces the efficiency of inspiration, leading to:
- Reduced tidal volume: This is the volume of air inhaled and exhaled with each breath. A smaller tidal volume means less oxygen is taken in and less carbon dioxide is expelled.
- Increased work of breathing: The weakened diaphragm has to work harder to achieve the same amount of ventilation, leading to increased fatigue and shortness of breath (dyspnea).
- Hypoxemia and hypercapnia: Reduced ventilation leads to lower oxygen levels in the blood (hypoxemia) and higher carbon dioxide levels (hypercapnia), which can have serious systemic consequences.
Intercostal and Accessory Muscle Weakness
The intercostal muscles located between the ribs also play a vital role in expanding the chest cavity during inspiration. Their weakness further compromises the efficiency of breathing, exacerbating the effects of diaphragmatic dysfunction. Similarly, the accessory muscles are recruited during increased respiratory effort, but their weakness in NMDs limits their ability to compensate for the weakened primary respiratory muscles. This results in:
- Increased respiratory rate: To compensate for reduced tidal volume, the respiratory rate often increases, leading to rapid, shallow breathing.
- Orthopnea: Difficulty breathing while lying down, often requiring the individual to sit or stand to breathe comfortably.
- Exercise intolerance: Even mild exertion can trigger significant shortness of breath due to the inability of the respiratory muscles to meet the increased demand for oxygen.
Beyond Respiratory Muscle Weakness: Other Contributing Factors
While respiratory muscle weakness is the primary cause of impaired lung function in NMDs, other factors contribute significantly:
Reduced Lung Volumes and Capacities
NMDs can affect lung volumes and capacities, representing the amount of air the lungs can hold and move. These changes are not merely a consequence of muscle weakness; they are also influenced by:
- Chest wall deformities: Some NMDs, such as Duchenne muscular dystrophy, can lead to skeletal muscle involvement, causing chest wall deformities like scoliosis (curvature of the spine) and kyphoscoliosis (combination of curvature and hunching). These deformities restrict chest expansion, reducing lung volumes and increasing the work of breathing.
- Reduced lung compliance: Compliance refers to the elasticity of the lungs. In NMDs, reduced lung compliance may result from reduced activity, leading to atelectasis (collapse of lung tissue) and reduced ability of the lungs to expand and contract efficiently.
- Respiratory infections: Weakness of the respiratory muscles and decreased cough effectiveness increase susceptibility to respiratory infections, which further impair lung function. Frequent infections can lead to chronic lung disease.
Impaired Cough Mechanism
A strong cough is essential for clearing secretions from the airways. Weakness of the abdominal and intercostal muscles, which are crucial for generating a forceful cough, severely impairs this mechanism in NMDs. This leads to:
- Increased risk of respiratory infections: Accumulation of secretions in the airways provides a breeding ground for bacteria and viruses.
- Atelectasis: Accumulation of secretions can lead to airway obstruction and collapse of lung tissue.
- Increased need for airway clearance techniques: Individuals with NMDs often require manual assisted coughing techniques or mechanical devices to help clear secretions.
Sleep-Disordered Breathing
NMDs significantly increase the risk of sleep-disordered breathing, specifically obstructive sleep apnea (OSA) and central sleep apnea (CSA).
- OSA is characterized by repeated episodes of upper airway obstruction during sleep, leading to pauses in breathing and reduced oxygen saturation. Weakness of the pharyngeal muscles, often present in NMDs, contributes to this obstruction.
- CSA involves the brain's failure to properly signal the respiratory muscles to breathe, leading to apnea episodes. This can be influenced by the underlying neurological involvement in some NMDs.
Sleep-disordered breathing further exacerbates hypoxemia and hypercapnia, leading to daytime sleepiness, cognitive impairment, and increased cardiovascular risk.
Specific Neuromuscular Disorders and Their Impact on Lung Function
The specific impact of NMDs on lung function varies depending on the underlying disorder.
Duchenne Muscular Dystrophy (DMD)
DMD is a progressive disorder primarily affecting skeletal muscles, including those involved in breathing. The progressive weakness of respiratory muscles leads to significant respiratory impairment, often necessitating ventilation support in later stages of the disease. Chest wall deformities such as scoliosis are common and contribute to further lung compromise.
Myasthenia Gravis (MG)
MG is an autoimmune disorder affecting the neuromuscular junction. While muscle weakness is fluctuating, it can significantly impact respiratory muscles, leading to respiratory failure, particularly during exacerbations. This emphasizes the importance of early diagnosis and management of MG.
Amyotrophic Lateral Sclerosis (ALS)
ALS is a progressive neurodegenerative disease affecting both upper and lower motor neurons. Respiratory muscle weakness is a hallmark of ALS and is a major determinant of prognosis. As the disease progresses, individuals often require non-invasive ventilation (NIV) or invasive mechanical ventilation to maintain adequate oxygenation.
Assessing and Managing Respiratory Impairment in NMDs
Early detection and management of respiratory impairment are crucial in NMDs to improve quality of life and prolong survival. Several assessments are used:
- Pulmonary function tests (PFTs): Measure lung volumes, capacities, and flow rates to assess the severity of respiratory impairment.
- Arterial blood gas analysis: Measures oxygen and carbon dioxide levels in the blood to determine the adequacy of gas exchange.
- Sleep studies: Diagnose and monitor sleep-disordered breathing.
- Electromyography (EMG): Assesses the electrical activity of muscles to evaluate the extent of muscle damage.
Management strategies vary depending on the severity of the respiratory impairment and the underlying NMD. These may include:
- Respiratory physiotherapy: Techniques to clear secretions, improve breathing patterns, and strengthen respiratory muscles.
- Non-invasive ventilation (NIV): Provides respiratory support without the need for tracheostomy.
- Invasive mechanical ventilation: Provides respiratory support through a tracheostomy.
- Medication: To treat respiratory infections and manage symptoms like cough and shortness of breath.
- Surgical intervention: To correct chest wall deformities.
Conclusion: A Holistic Approach
Neuromuscular disorders impair lung function primarily due to respiratory muscle weakness, but this is further exacerbated by chest wall deformities, impaired cough mechanisms, and increased susceptibility to respiratory infections. The resulting respiratory insufficiency significantly impacts the quality of life and prognosis of individuals with NMDs. A holistic approach, encompassing regular monitoring of lung function, early intervention with respiratory support, and management of associated complications, is essential to optimize respiratory health and improve outcomes for those living with these challenging conditions. Early diagnosis, proactive management, and comprehensive care plans are crucial for improving the respiratory health and overall well-being of individuals affected by NMDs. Further research into the pathophysiology of respiratory compromise in NMDs is necessary to develop novel and effective therapies.
Latest Posts
Latest Posts
-
Lesson 3 4 Solving Complex 1 Variable Equations Answer Key
Mar 04, 2025
-
Song Chart Bars Dear No One By Tori Kelly
Mar 04, 2025
-
Death Row Contract Relationship Copy And Paste
Mar 04, 2025
-
Cpi Test Questions And Answers Pdf
Mar 04, 2025
-
Identify Steps In Building A Fire
Mar 04, 2025
Related Post
Thank you for visiting our website which covers about Neuromuscular Disorders Impair Lung Function Primarily Because Of . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
