Nursing Care Plan For Neonatal Jaundice
Onlines
Apr 03, 2025 · 6 min read
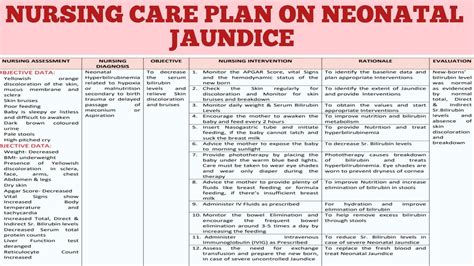
Table of Contents
- Nursing Care Plan For Neonatal Jaundice
- Table of Contents
- Nursing Care Plan for Neonatal Jaundice
- Understanding Neonatal Jaundice
- Types of Neonatal Jaundice
- Risk Factors for Neonatal Jaundice
- Nursing Assessment for Neonatal Jaundice
- 1. History Taking
- 2. Physical Examination
- 3. Laboratory Investigations
- Nursing Interventions for Neonatal Jaundice
- 1. Monitoring Bilirubin Levels
- 2. Phototherapy
- 3. Exchange Transfusion
- 4. Supportive Care
- Nursing Evaluation
- Preventing Complications
- Conclusion
- Latest Posts
- Latest Posts
- Related Post
Nursing Care Plan for Neonatal Jaundice
Neonatal jaundice, a common condition affecting newborns, is characterized by yellowing of the skin and whites of the eyes due to a buildup of bilirubin. While often benign and resolving spontaneously, it's crucial to understand the nuances of nursing care to ensure timely detection, appropriate management, and prevention of potential complications. This comprehensive guide provides a detailed nursing care plan for neonatal jaundice, encompassing assessment, interventions, and evaluation.
Understanding Neonatal Jaundice
Before delving into the care plan, let's establish a firm understanding of neonatal jaundice. Bilirubin, a byproduct of the breakdown of hemoglobin, is normally processed and excreted by the liver. In newborns, the immature liver may struggle to efficiently conjugate and eliminate bilirubin, leading to its accumulation in the bloodstream. This hyperbilirubinemia manifests as jaundice.
Types of Neonatal Jaundice
Neonatal jaundice is broadly classified into two types based on the timing of onset:
-
Physiological Jaundice: This is the most common type, typically appearing after 24 hours of life and resolving within 2 weeks. It's often attributed to the normal physiological processes of bilirubin metabolism in the newborn.
-
Pathological Jaundice: This type appears within the first 24 hours of life or persists beyond 2 weeks. It indicates an underlying medical condition, such as hemolytic disease, infection, or liver dysfunction. Pathological jaundice requires prompt medical intervention.
Risk Factors for Neonatal Jaundice
Several factors increase a newborn's risk of developing jaundice:
- Prematurity: Premature infants have immature livers and are at higher risk.
- Cephalhematoma: This collection of blood under the scalp can lead to increased bilirubin levels.
- Bruising: Extensive bruising during birth can contribute to jaundice.
- Breastfeeding: While breastfeeding is beneficial, certain factors related to breastfeeding can sometimes contribute to jaundice. This is often termed breastfeeding-associated jaundice.
- ABO or Rh incompatibility: Blood type incompatibility between the mother and baby can cause hemolytic disease of the newborn, leading to increased bilirubin levels.
- Genetic factors: Certain genetic conditions can increase the risk of jaundice.
- Infection: Infections can contribute to increased bilirubin production.
- Hypothyroidism: Underactive thyroid function can impair bilirubin metabolism.
Nursing Assessment for Neonatal Jaundice
A thorough assessment is fundamental to effective management. The nursing assessment should include:
1. History Taking
- Maternal history: Assess the mother's blood type, history of previous pregnancies, and any complications during pregnancy or labor.
- Birth history: Note the gestational age, birth weight, and any signs of trauma or infection during birth.
- Feeding history: Determine the type of feeding (breastfeeding or formula feeding) and the infant's feeding pattern.
- Family history: Inquire about any family history of jaundice.
2. Physical Examination
- Skin assessment: Observe the extent and progression of jaundice. The classic progression is from head to toe, starting with the face and extending downwards. Document the location and intensity of jaundice using a standardized scale, such as the Kramer scale.
- Vital signs: Monitor heart rate, respiratory rate, temperature, and blood pressure.
- Neurological assessment: Assess for signs of bilirubin encephalopathy (kernicterus), such as lethargy, poor feeding, hypotonia, and high-pitched cry.
- Assessment of hydration: Observe for signs of dehydration, such as sunken fontanelles, dry mucous membranes, and decreased urine output.
3. Laboratory Investigations
- Total serum bilirubin (TSB): This is the primary laboratory test used to assess the severity of jaundice. Levels are typically measured using transcutaneous bilirubinometry (TcB) or by drawing blood samples for laboratory analysis. The appropriate management strategy often depends on the TSB level in conjunction with the infant's age and gestational age.
- Direct and indirect bilirubin: This helps differentiate between conjugated and unconjugated bilirubin. Elevated levels of indirect bilirubin are more commonly associated with neonatal jaundice.
- Complete blood count (CBC): This helps assess for hemolysis or infection.
- Blood type and Rh factor: Determine the blood group compatibility between the mother and infant.
- Coombs test: This test checks for antibodies that may be causing hemolytic disease.
- Liver function tests: Assess liver function, particularly in cases of suspected liver disease.
Nursing Interventions for Neonatal Jaundice
Nursing interventions focus on minimizing bilirubin levels, preventing complications, and providing supportive care.
1. Monitoring Bilirubin Levels
- Regular monitoring: Frequent monitoring of bilirubin levels using TcB or serum bilirubin measurements is crucial, especially in high-risk infants. The frequency of monitoring is determined by the infant’s risk factors and the initial bilirubin level.
- Accurate documentation: Meticulously document bilirubin levels, along with the timing and method of measurement.
2. Phototherapy
Phototherapy is a primary treatment for neonatal jaundice. It involves exposing the infant to special lights that convert bilirubin into a water-soluble form, which can be excreted.
- Preparation: Ensure the infant's eyes are protected with eye patches to prevent retinal damage. Remove the eye patches during feedings and brief periods for skin assessment.
- Positioning: Regularly reposition the infant to ensure even exposure to the lights and to prevent pressure sores.
- Fluid intake: Encourage frequent feeding to help excrete bilirubin through the urine and stool. Closely monitor the infant's hydration status.
- Skin assessment: Assess the infant's skin for any signs of burns or dehydration. Maintain a neutral thermal environment to avoid temperature extremes.
- Monitoring: Carefully monitor the infant's temperature, vital signs, and urine output during phototherapy.
3. Exchange Transfusion
In severe cases of jaundice, an exchange transfusion may be necessary. This procedure involves removing the infant's blood and replacing it with fresh donor blood to rapidly reduce bilirubin levels.
- Pre-procedure care: Accurate monitoring of vital signs and careful assessment for signs of bilirubin encephalopathy are crucial.
- Post-procedure care: Closely monitor the infant's vital signs, hydration status, and blood glucose levels.
4. Supportive Care
- Feeding: Frequent feedings are essential to promote bilirubin excretion. Breastfeeding is encouraged as long as the infant is gaining weight appropriately. Supplemental feedings may be necessary to maintain hydration.
- Hydration: Monitor fluid intake and output meticulously. Infants with dehydration should receive appropriate intravenous fluids.
- Skin care: Protect the infant's skin from dryness and irritation. Use gentle cleansers and moisturizers as needed.
- Comfort: Provide a calm and soothing environment. Use swaddling, cuddling, and skin-to-skin contact to provide comfort.
- Education: Provide comprehensive education to the parents about neonatal jaundice, its management, and the importance of follow-up care.
Nursing Evaluation
Ongoing evaluation is crucial to ensure the effectiveness of the nursing interventions. This involves:
- Monitoring bilirubin levels: Regularly monitor bilirubin levels to assess the response to treatment.
- Assessing clinical signs: Observe for any improvement in the infant's skin color, behavior, and overall condition.
- Evaluating parental understanding: Assess the parents' understanding of the condition and the treatment plan.
- Documenting progress: Maintain meticulous documentation of all assessments, interventions, and the infant's response to treatment.
Preventing Complications
Early detection and appropriate management are key to preventing complications associated with neonatal jaundice. Complications can include:
- Bilirubin encephalopathy (kernicterus): This is a serious neurological condition caused by high levels of bilirubin that can lead to permanent brain damage.
- Hearing loss: High bilirubin levels can affect hearing.
- Cerebral palsy: In severe cases, jaundice can contribute to cerebral palsy.
- Death: In untreated severe cases, jaundice can be fatal.
Conclusion
Neonatal jaundice is a common condition requiring a comprehensive and individualized nursing care plan. Early detection, accurate assessment, and prompt interventions are essential to prevent complications and ensure the best possible outcome for the newborn. Close collaboration between nurses, physicians, and parents is crucial for successful management and positive parental experiences. This holistic approach emphasizes the importance of education, individualized plans, and vigilant monitoring in promoting the well-being of newborns affected by neonatal jaundice. Remember that this information is for educational purposes only and should not replace professional medical advice. Always consult with a healthcare provider for diagnosis and treatment.
Latest Posts
Latest Posts
-
Chapter 17 Concepts Of Care For Patients With Hiv Disease
Apr 08, 2025
-
Keshawn Used To Work For An It Company In Baltimore
Apr 08, 2025
-
A Patient With Hypertension Receives A Prescription For Lisinopril
Apr 08, 2025
-
Yo Les Envie Postales A Mis Amigos
Apr 08, 2025
-
Big 10 Composition Of Functions Topic 2 7
Apr 08, 2025
Related Post
Thank you for visiting our website which covers about Nursing Care Plan For Neonatal Jaundice . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.