Paralytic Medications Exert Their Effect By
Onlines
Apr 01, 2025 · 6 min read
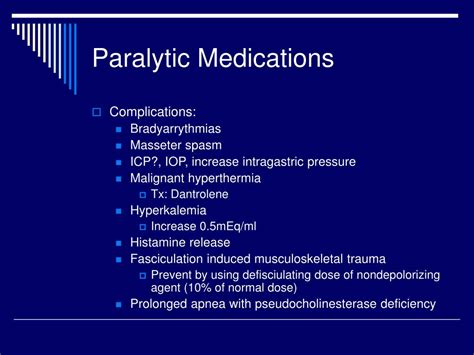
Table of Contents
Paralytic Medications: Mechanisms of Action and Clinical Applications
Paralytic medications, also known as neuromuscular blocking agents (NMBAs), are a class of drugs that temporarily paralyze skeletal muscles. Their effects are achieved by interfering with the neuromuscular junction, the specialized synapse where motor neurons transmit signals to muscle fibers. Understanding how these medications exert their effects is crucial for safe and effective clinical application, especially in anesthesia, critical care, and other specialized medical fields. This comprehensive article will explore the diverse mechanisms by which paralytic medications achieve their effects, delve into their clinical uses, and discuss important considerations regarding their administration and potential side effects.
Mechanisms of Action: Disrupting Neuromuscular Transmission
Paralytic medications primarily act by interfering with the transmission of nerve impulses at the neuromuscular junction. This junction is a complex interplay of presynaptic nerve terminals, the synaptic cleft, and postsynaptic muscle fibers. The process of muscle contraction involves the release of acetylcholine (ACh), a neurotransmitter, from the presynaptic nerve terminal. ACh then binds to nicotinic acetylcholine receptors (nAChRs) located on the postsynaptic muscle membrane, initiating a cascade of events leading to muscle fiber depolarization and contraction. NMBAs disrupt this process in different ways, broadly categorized into two main groups:
1. Depolarizing Neuromuscular Blocking Agents (Succinylcholine):
Succinylcholine is the only clinically used depolarizing NMBA. It uniquely mimics the action of acetylcholine.
-
Mechanism: Succinylcholine binds to the nAChRs on the muscle membrane, causing depolarization and initial muscle fasciculations (brief, involuntary muscle contractions). However, unlike ACh, succinylcholine is not rapidly metabolized by acetylcholinesterase. This prolonged depolarization leads to a sustained inactivation of the nAChRs, preventing further muscle contraction and resulting in paralysis. The receptor remains occupied and unable to respond to subsequent ACh release.
-
Clinical Implications: The rapid onset and short duration of action make succinylcholine suitable for short procedures like intubation. However, its unique mechanism also contributes to potential side effects, such as hyperkalemia (elevated potassium levels), particularly in patients with pre-existing conditions like burns or muscle injury. Malignant hyperthermia, a rare but life-threatening complication, is also a concern. Repeated doses can cause desensitization of the receptors.
2. Non-Depolarizing Neuromuscular Blocking Agents:
This larger group comprises various medications that competitively antagonize the action of acetylcholine at the nAChRs.
-
Mechanism: Non-depolarizing NMBAs bind competitively to the nAChRs on the postsynaptic muscle membrane, preventing ACh from binding and initiating muscle contraction. This competitive antagonism results in a graded response; increasing doses lead to progressively greater muscle paralysis.
-
Subtypes & Clinical Characteristics: Non-depolarizing NMBAs are further classified into several subtypes based on their chemical structure and duration of action:
-
Benzylisoquinolinium compounds (e.g., atracurium, cisatracurium, mivacurium): These agents are known for their relatively short durations of action and are often preferred for shorter procedures. They undergo spontaneous degradation in the body.
-
Steroidal compounds (e.g., rocuronium, vecuronium, pancuronium): These medications generally have longer durations of action compared to benzylisoquinolinium compounds, making them suitable for longer surgical procedures or critical care situations. They are eliminated primarily through the liver and kidneys.
-
Aminosteroid compounds (e.g., rapacuronium): This class offers a unique profile with characteristics that vary across different agents.
-
The specific choice of a non-depolarizing NMBA depends on factors such as the duration of the procedure, patient characteristics, and potential drug interactions.
Clinical Applications: A Wide Range of Uses
Paralytic medications play a vital role in various medical specialties, including:
1. Anesthesia:
-
Facilitating Endotracheal Intubation: NMBAs are essential for securing an airway during anesthesia. They induce muscle relaxation, allowing for easier and safer intubation.
-
Surgical Relaxation: By providing skeletal muscle relaxation, they facilitate surgical procedures, reducing the risk of muscle injury and improving surgical access.
-
Mechanical Ventilation: In patients requiring mechanical ventilation, NMBAs can help to synchronize breathing with the ventilator and improve gas exchange.
2. Critical Care:
-
Intubation and Mechanical Ventilation: Similar to their role in anesthesia, NMBAs aid in managing airways and facilitating mechanical ventilation in critically ill patients.
-
Status Epilepticus: In cases of prolonged seizures (status epilepticus), NMBAs can help to protect the patient from self-injury caused by uncontrolled muscle activity.
-
Reduction of Intracranial Pressure: In patients with increased intracranial pressure, muscle relaxation can help to decrease metabolic demand and reduce the risk of further pressure elevation.
3. Other Applications:
-
Electroconvulsive Therapy (ECT): NMBAs are commonly used during ECT to minimize muscle contractions and prevent injuries.
-
Diagnostic Procedures: In certain diagnostic procedures, muscle relaxation is required. NMBAs can help in this regard.
-
Management of Spasticity: In specific situations, NMBAs can help manage muscle spasms and spasticity associated with neurological conditions.
Reversal Agents: Countering the Effects of NMBAs
The effects of NMBAs are typically reversible. Specific drugs called reversal agents can help restore neuromuscular function after the NMBA's effect has subsided or been terminated. The most commonly used reversal agent is neostigmine.
-
Neostigmine Mechanism: This drug inhibits acetylcholinesterase, the enzyme that breaks down acetylcholine. By increasing the concentration of ACh at the neuromuscular junction, it competes with non-depolarizing NMBAs and restores neuromuscular transmission. It's typically used in conjunction with atropine, which counteracts the muscarinic side effects of neostigmine.
-
Edrophonium: Another cholinesterase inhibitor, edrophonium, has a shorter duration of action compared to neostigmine and can be helpful in assessing residual neuromuscular blockade.
The timing and dose of the reversal agent are crucial and should be carefully determined based on the specific NMBA used, the patient's clinical condition, and the assessment of neuromuscular function using techniques such as the train-of-four stimulation.
Adverse Effects and Monitoring: Ensuring Patient Safety
While crucial for many medical procedures, paralytic medications are not without potential adverse effects. Careful monitoring and management are essential to minimize risks.
-
Respiratory Depression: This is the most significant adverse effect, as NMBAs can paralyze the respiratory muscles, leading to respiratory failure. Mechanical ventilation is essential when using these medications.
-
Hypotension: Some NMBAs can cause a drop in blood pressure, which must be managed appropriately.
-
Cardiac Arrhythmias: Certain NMBAs can have effects on the heart, potentially causing arrhythmias.
-
Hyperkalemia: Particularly with succinylcholine, there is a risk of increased potassium levels in the blood, potentially dangerous for patients with pre-existing conditions.
-
Malignant Hyperthermia: This rare but potentially fatal condition can be triggered by succinylcholine in susceptible individuals.
-
Allergic Reactions: Although rare, allergic reactions are possible.
Continuous monitoring of vital signs, including respiratory rate, blood pressure, heart rate, and oxygen saturation, is crucial during the administration of NMBAs. Assessment of neuromuscular function using methods like train-of-four stimulation allows for the precise determination of the degree of paralysis and helps guide the administration of reversal agents.
Conclusion: Precision and Patient Safety
Paralytic medications are powerful tools with important applications in various medical specialties. Their ability to temporarily paralyze skeletal muscles offers significant benefits in procedures ranging from airway management to complex surgeries. However, their potent effects necessitate careful understanding of their mechanisms of action, potential side effects, and the crucial role of monitoring and the appropriate use of reversal agents. By adhering to strict guidelines and employing meticulous patient monitoring, healthcare professionals can leverage the advantages of these medications while minimizing the risks and ensuring patient safety. Further research continues to refine our understanding of NMBAs, leading to the development of newer agents with improved profiles and fewer side effects. The future of paralytic medications involves a delicate balance between enhanced efficacy and minimizing the risks associated with their profound effect on neuromuscular function.
Latest Posts
Latest Posts
-
Within The Context Of Rcr Social Responsibility Primarily Refers To
Apr 02, 2025
-
General Purpose Applications Include All The Following Except
Apr 02, 2025
-
Dad 220 Module 6 Project One
Apr 02, 2025
-
Advanced Hardware Lab 8 3 Select And Install Network Hardware
Apr 02, 2025
-
Where Is The Value Of A Raw Material Tracked
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Paralytic Medications Exert Their Effect By . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
