Procedure 1 Tracing Substances Through The Kidney
Onlines
Mar 29, 2025 · 6 min read
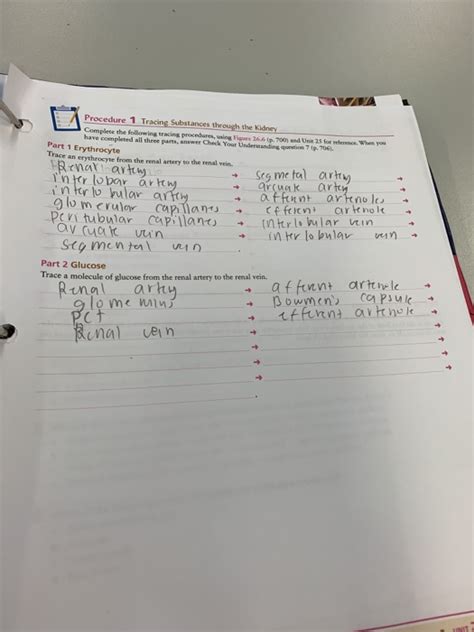
Table of Contents
Procedure 1: Tracing Substances Through the Kidney
Understanding how the kidneys filter and process substances is fundamental to comprehending human physiology and diagnosing various renal diseases. This detailed exploration of Procedure 1—tracing substances through the kidney—will delve into the intricate mechanisms involved, utilizing a step-by-step approach to clarify the process. We'll examine different substances and their unique pathways, highlighting the roles of key structures like the glomerulus, Bowman's capsule, proximal convoluted tubule, loop of Henle, distal convoluted tubule, and collecting duct. We'll also explore how this procedure helps in diagnosing kidney function and identifying potential problems.
Understanding Renal Function: A Quick Overview
Before delving into the specifics of Procedure 1, a brief review of fundamental renal functions is crucial. The kidneys are vital organs primarily responsible for:
- Filtration: Removing waste products and excess fluid from the blood.
- Reabsorption: Reclaiming essential substances like glucose, amino acids, and water that were initially filtered.
- Secretion: Actively transporting specific substances from the blood into the tubules for excretion.
- Excretion: Eliminating waste products and excess substances from the body through urine.
These four processes work in concert to maintain the body's internal environment (homeostasis), regulating blood pressure, electrolyte balance, and pH.
Procedure 1: Step-by-Step Tracing of Substances
Procedure 1 involves tracking the movement of a substance (e.g., inulin, creatinine, glucose, PAH – para-aminohippuric acid) as it travels through the nephron, the functional unit of the kidney. This process helps determine the glomerular filtration rate (GFR), renal plasma flow (RPF), and the specific handling of different substances by the kidney.
Step 1: Glomerular Filtration
The journey begins at the glomerulus, a network of capillaries within Bowman's capsule. Here, blood pressure forces water and small solutes (substances dissolved in the water) from the glomerular capillaries into the Bowman's space. This process is non-selective, meaning that most substances smaller than a certain size (around 70 kDa) are filtered. Larger molecules like proteins typically remain in the blood. The filtrate entering Bowman's capsule is similar to blood plasma but lacks large proteins.
Substances traced: Inulin, creatinine, glucose, PAH. All pass through the glomerular membrane (with varying efficiency) unless bound to plasma proteins.
Step 2: Proximal Convoluted Tubule (PCT)
The filtrate then flows into the proximal convoluted tubule (PCT). This section of the nephron is responsible for the majority of reabsorption. Here, essential substances like glucose, amino acids, water, sodium, potassium, bicarbonate, and chloride are actively or passively transported back into the bloodstream. Some substances undergo secretion here as well – drugs and toxins are actively transported from the peritubular capillaries into the PCT lumen.
Substances traced:
- Glucose: Almost completely reabsorbed via secondary active transport coupled with sodium reabsorption.
- Amino acids: Almost completely reabsorbed via secondary active transport.
- Inulin: Not reabsorbed or secreted; its concentration remains relatively constant throughout the nephron, making it an excellent marker for GFR.
- Creatinine: Mostly filtered, small amount secreted. Some reabsorption occurs, but it is minimal.
- PAH: Freely filtered and almost completely secreted in the PCT, making it a good marker for RPF.
Step 3: Loop of Henle
The filtrate then enters the loop of Henle, a U-shaped structure crucial for establishing a concentration gradient in the renal medulla. The descending limb is permeable to water, while the ascending limb is impermeable to water but actively transports sodium and chloride ions out of the filtrate. This countercurrent mechanism concentrates the filtrate in the medulla and plays a vital role in urine concentration.
Substances traced:
- Inulin: Remains unchanged in concentration.
- Creatinine: Minimal changes; mostly unchanged.
- Glucose: Essentially absent due to complete reabsorption in the PCT.
- PAH: Concentration decreases due to continuing secretion in the early parts of the loop of Henle
Step 4: Distal Convoluted Tubule (DCT)
The filtrate moves from the loop of Henle into the distal convoluted tubule (DCT). Fine-tuning of electrolyte and pH balance occurs here. Reabsorption of sodium and calcium (regulated by hormones like parathyroid hormone and aldosterone) and secretion of potassium and hydrogen ions take place.
Substances traced:
- Inulin: Remains unchanged in concentration.
- Creatinine: Minimal changes; mostly unchanged.
- Glucose: Absent.
- PAH: Concentration changes minimally as the majority of secretion happened in the PCT
Step 5: Collecting Duct
Finally, the filtrate enters the collecting duct, where the final adjustments to urine concentration and composition take place. The permeability of the collecting duct to water is regulated by antidiuretic hormone (ADH), allowing for the fine control of water reabsorption and urine concentration.
Substances traced:
- Inulin: Remains unchanged, providing a final measure of GFR.
- Creatinine: Minimal changes, reflecting the total excretion.
- Glucose: Absent, unless there's glucosuria (glucose in the urine).
- PAH: Concentration reflects the total renal clearance, providing an indication of RPF.
Clinical Significance of Procedure 1
Procedure 1, while theoretical, forms the basis of several clinical tests that assess kidney function. By measuring the concentration of different substances in the blood and urine, clinicians can:
-
Determine Glomerular Filtration Rate (GFR): Inulin clearance is the gold standard for measuring GFR, representing the volume of plasma filtered by the glomeruli per unit time. Creatinine clearance is often used as a clinical approximation of GFR, being readily measurable in blood and urine samples. A low GFR indicates reduced kidney function.
-
Assess Renal Plasma Flow (RPF): PAH clearance provides a measure of RPF, indicating the volume of plasma flowing through the kidneys per unit time. Reduced RPF can signify impaired renal blood flow.
-
Detect Renal Tubular Dysfunction: Analyzing the urinary excretion of substances like glucose (glycosuria), amino acids (aminoaciduria), and proteins (proteinuria) can reveal abnormalities in tubular reabsorption or secretion. This is crucial in diagnosing various renal diseases.
-
Monitor Kidney Disease Progression: Regular monitoring of GFR and other parameters allows for the effective management and tracking of kidney disease progression.
-
Evaluate the effectiveness of treatments: changes in GFR, RPF, and urinary excretion of specific substances can be used to monitor the response to various treatments for kidney diseases.
Further Considerations and Applications
While the simplified step-by-step approach offers a clear understanding of the process, many complexities are involved in real-world renal function. Hormonal regulation, interactions between different substances, and the influence of various diseases add significant layers of nuance.
The concept of clearance is central to Procedure 1. Clearance refers to the volume of plasma that is completely cleared of a substance per unit time. Different substances have varying clearance rates due to differences in filtration, reabsorption, and secretion.
Moreover, Procedure 1 lays the foundation for understanding more complex renal processes, such as:
- Acid-base balance: The kidneys play a crucial role in maintaining blood pH through the secretion of hydrogen ions and reabsorption of bicarbonate.
- Electrolyte balance: The kidneys regulate the concentration of electrolytes like sodium, potassium, calcium, and phosphate in the blood.
- Blood pressure regulation: The kidneys contribute to blood pressure regulation through the renin-angiotensin-aldosterone system.
Conclusion
Procedure 1: tracing substances through the kidney is a fundamental concept in renal physiology. By following the movement of different substances through the nephron, we gain valuable insights into the intricate mechanisms of filtration, reabsorption, secretion, and excretion. This understanding forms the bedrock of clinical tests used to diagnose and monitor kidney function, enabling early detection and effective management of renal diseases. The detailed examination of this procedure allows for a comprehensive appreciation of the vital role the kidneys play in maintaining homeostasis and overall health. This process, while described in a simplified manner, highlights the remarkable complexity and efficiency of the human renal system. Continued research into this intricate system promises further advancements in understanding and treating kidney diseases.
Latest Posts
Latest Posts
-
Which Comparison Contrast Statement Is Most Effective
Apr 01, 2025
-
Gizmo Student Exploration Unit Conversions Answer Key
Apr 01, 2025
-
Which Sequence Of Transformation Carries Abcd Onto Efgh
Apr 01, 2025
-
Eaps 105 Exam 1 Study Guide
Apr 01, 2025
-
Floral Design Basics Principles And Elements
Apr 01, 2025
Related Post
Thank you for visiting our website which covers about Procedure 1 Tracing Substances Through The Kidney . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
