Pulmonary Edema And Impaired Ventilation Occur During:
Onlines
Apr 01, 2025 · 6 min read
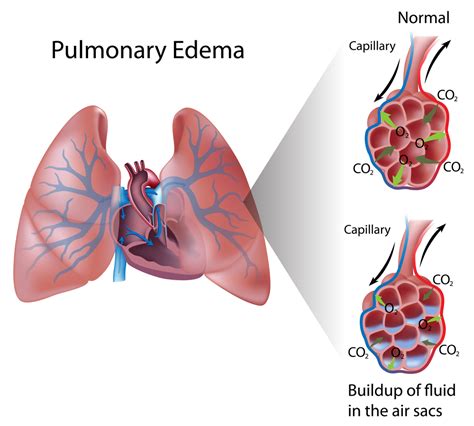
Table of Contents
Pulmonary Edema and Impaired Ventilation: A Comprehensive Overview
Pulmonary edema, characterized by fluid accumulation in the air sacs of the lungs, and impaired ventilation, a reduction in the efficiency of gas exchange, frequently occur together, significantly impacting respiratory function. Understanding the underlying mechanisms and the conditions leading to this dangerous combination is crucial for effective diagnosis and management. This article delves into the various scenarios where pulmonary edema and impaired ventilation are concurrently observed, exploring their causes, consequences, and clinical implications.
Understanding the Interplay Between Pulmonary Edema and Impaired Ventilation
Pulmonary edema disrupts the normal gas exchange process. The fluid buildup in the alveoli interferes with the diffusion of oxygen into the bloodstream and carbon dioxide out of the bloodstream. This impaired diffusion leads to hypoxemia (low blood oxygen levels) and hypercapnia (elevated blood carbon dioxide levels), both critical signs of respiratory distress. Simultaneously, impaired ventilation, stemming from various causes, further exacerbates the situation. The reduced ability to adequately ventilate the lungs worsens the hypoxemia and hypercapnia, leading to a vicious cycle of respiratory compromise.
Conditions Leading to Concurrent Pulmonary Edema and Impaired Ventilation
Several conditions can trigger the simultaneous occurrence of pulmonary edema and impaired ventilation. These conditions often share overlapping mechanisms that contribute to both fluid buildup in the lungs and compromised ventilation. Let's explore some of the most prominent:
1. Acute Respiratory Distress Syndrome (ARDS)
ARDS is a severe lung injury characterized by widespread inflammation and fluid leakage into the alveoli. This leads to both pulmonary edema and significant impairment of ventilation due to the widespread alveolar damage and reduced lung compliance (the ability of the lungs to expand). The inflammatory process itself can also impair ventilation by causing bronchoconstriction (narrowing of the airways). ARDS can result from various causes, including:
- Sepsis: A systemic inflammatory response to infection.
- Pneumonia: Infection of the lung tissue.
- Aspiration: Inhaling foreign substances into the lungs.
- Trauma: Significant injury, particularly chest trauma.
- Pancreatitis: Inflammation of the pancreas.
- Drug overdose: Certain medications can trigger ARDS.
2. Cardiogenic Pulmonary Edema
Cardiogenic pulmonary edema is the most common type of pulmonary edema, resulting from left-sided heart failure. The weakened heart struggles to pump blood effectively, leading to increased pressure in the pulmonary capillaries (blood vessels in the lungs). This elevated pressure forces fluid into the surrounding alveoli, causing pulmonary edema. While the primary issue is fluid buildup, impaired ventilation can occur due to:
- Compression of alveoli: The fluid buildup itself physically compresses the alveoli, hindering their ability to expand and participate in gas exchange.
- Increased airway resistance: Fluid accumulation can obstruct smaller airways, increasing the resistance to airflow.
- Atelectasis: Collapse of alveoli due to the fluid accumulation.
Furthermore, the underlying heart condition can independently affect ventilation, as reduced cardiac output can lead to decreased tissue perfusion and overall compromised oxygen delivery.
3. High-Altitude Pulmonary Edema (HAPE)
HAPE occurs at high altitudes due to the low partial pressure of oxygen. The body's response to hypoxia (low oxygen levels) includes increased pulmonary blood flow, which, combined with increased permeability of the pulmonary capillaries, leads to fluid leakage into the alveoli. This is accompanied by impaired ventilation due to:
- Hypoxic vasoconstriction: The body attempts to shunt blood away from poorly ventilated areas, but this can lead to uneven distribution of blood flow in the lungs, further hindering gas exchange.
- Alveolar collapse: Hypoxia can cause alveolar collapse, further reducing the surface area available for gas exchange.
The combination of fluid buildup and impaired ventilation significantly reduces oxygen uptake, creating a life-threatening situation.
4. Near-Drowning
Near-drowning incidents often lead to both pulmonary edema and impaired ventilation. The aspiration of water into the lungs causes direct injury to the alveoli, leading to fluid accumulation and inflammation. Furthermore, the physical effects of aspiration, including airway obstruction and alveolar collapse, cause significant impairment of ventilation. The resulting hypoxia and hypercapnia can cause severe complications, including brain damage and cardiac arrest.
5. Pneumonia
Pneumonia, an infection of the lung parenchyma, can lead to pulmonary edema through several mechanisms. The inflammatory process causes increased capillary permeability, leading to fluid leakage into the alveoli. Furthermore, the accumulation of inflammatory exudate and mucus can obstruct airways, significantly impairing ventilation. The infection itself can cause alveolar collapse and reduce lung compliance.
6. Inhalation Injuries
Inhalation of toxic fumes, smoke, or other irritants can cause severe lung injury, resulting in acute respiratory distress. The irritants directly damage the alveoli, causing inflammation and increased capillary permeability. This leads to fluid leakage and pulmonary edema. Simultaneously, the inflammation and bronchoconstriction caused by the irritants significantly impair ventilation.
Clinical Manifestations
The clinical presentation of concurrent pulmonary edema and impaired ventilation varies depending on the underlying cause and severity. However, common features include:
- Dyspnea (shortness of breath): Often severe and progressive.
- Tachypnea (rapid breathing): The body attempts to compensate for hypoxemia.
- Tachycardia (rapid heart rate): A compensatory response to hypoxemia and reduced blood pressure.
- Hypoxemia: Low blood oxygen levels, detected through pulse oximetry or arterial blood gas analysis.
- Hypercapnia: Elevated blood carbon dioxide levels, also detected through arterial blood gas analysis.
- Cough: May be productive (with sputum) or non-productive.
- Crackles (rales): Abnormal lung sounds heard during auscultation, indicating fluid in the alveoli.
- Wheezing: May be present if bronchospasm is a contributing factor.
- Cyanosis: Bluish discoloration of the skin and mucous membranes due to low oxygen saturation.
Diagnosis and Management
Accurate diagnosis involves a combination of clinical evaluation, imaging studies, and laboratory tests. Chest X-ray is crucial for visualizing the extent of pulmonary edema. Arterial blood gas analysis provides crucial information on oxygen and carbon dioxide levels. Echocardiography may be necessary to evaluate cardiac function in cases of suspected cardiogenic pulmonary edema. Other investigations may include CT scans, bronchoscopy, and various blood tests.
Management focuses on supporting respiratory function and addressing the underlying cause. Treatment may include:
- Oxygen therapy: To increase blood oxygen levels.
- Mechanical ventilation: In severe cases, to assist breathing.
- Positive end-expiratory pressure (PEEP): A technique used in mechanical ventilation to keep the alveoli open.
- Diuretics: To remove excess fluid in cases of cardiogenic pulmonary edema.
- Treatment of the underlying cause: Addressing infections (with antibiotics), managing heart failure, or providing supportive care for other conditions.
Prognosis and Prevention
The prognosis for patients with concurrent pulmonary edema and impaired ventilation depends largely on the underlying cause, severity, and promptness of treatment. Early diagnosis and aggressive management are crucial for improving outcomes. Prevention strategies focus on avoiding or managing risk factors, such as controlling hypertension, managing heart failure, avoiding smoking, and preventing infections.
Conclusion
Pulmonary edema and impaired ventilation often occur together, representing a significant respiratory challenge. Understanding the underlying mechanisms and the variety of conditions that lead to this dangerous combination is crucial for effective diagnosis and management. This article has provided a comprehensive overview, highlighting the interplay between these conditions and the importance of prompt medical intervention for improved patient outcomes. Further research continues to advance our understanding and refine treatment strategies for these life-threatening conditions.
Latest Posts
Latest Posts
-
Ionic Bonding Puzzle Activity Answer Key
Apr 02, 2025
-
Cash Reconciliations Can Be Tested Via
Apr 02, 2025
-
Distance Midpoint And Angle Measurement Embedded Assessment 2 Answers
Apr 02, 2025
-
What Are The Themes Of Julius Caesar
Apr 02, 2025
-
The Lottery By Shirley Jackson Characters
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Pulmonary Edema And Impaired Ventilation Occur During: . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
