Respiratory System Hourly Rounds Shadow Health Richard
Onlines
Mar 15, 2025 · 6 min read
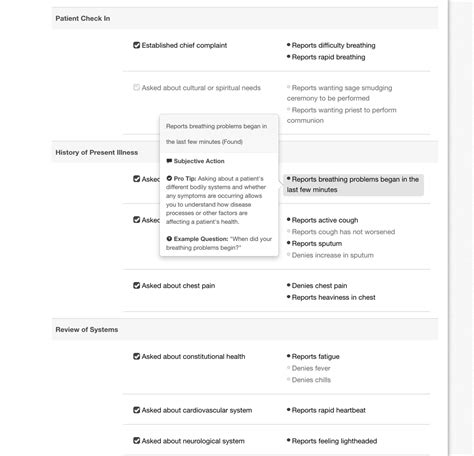
Table of Contents
Respiratory System Hourly Rounds: Mastering the Shadow Health Assessment
Shadow Health's interactive patient simulations provide invaluable training for healthcare professionals. This in-depth guide focuses on effectively performing respiratory system hourly rounds within the Shadow Health Richard simulation, covering crucial assessment techniques, potential pitfalls, and strategies for optimal performance. We'll explore the importance of thorough observation, precise questioning, and skillful interpretation of findings. Mastering these skills will enhance your diagnostic accuracy and patient care capabilities.
Understanding the Context of Hourly Rounds
Hourly rounds are crucial for patients with respiratory compromise. These frequent assessments allow for early detection of subtle changes in respiratory status, enabling prompt intervention and preventing potentially life-threatening complications. Richard, in the Shadow Health simulation, might present with various respiratory conditions requiring vigilant monitoring. Your success hinges on your ability to identify deteriorating respiratory function early.
Key Objectives of Hourly Respiratory Assessments:
- Early Detection of Deterioration: Identifying worsening respiratory distress before it becomes critical.
- Monitoring Treatment Effectiveness: Assessing the impact of interventions like oxygen therapy, medications, or respiratory support.
- Preventing Complications: Proactively addressing issues such as hypoxemia, hypercapnia, or respiratory infections.
- Patient Education and Empowerment: Reinforcing understanding of their condition and encouraging active participation in their care.
- Documentation: Meticulously recording observations and interventions for continuity of care.
Essential Elements of a Comprehensive Respiratory Assessment
A thorough hourly respiratory assessment in Shadow Health Richard (or any similar simulation) must integrate several key components:
1. Observation: The Silent Storyteller
Before initiating direct interaction, carefully observe Richard. This non-verbal assessment provides valuable clues. Look for:
- Respiratory Rate and Rhythm: Is the breathing rate within normal limits (12-20 breaths per minute)? Is the rhythm regular or irregular (e.g., Cheyne-Stokes breathing, Kussmaul breathing)? Observe for tachypnea (rapid breathing) or bradypnea (slow breathing). Note any use of accessory muscles (e.g., intercostal retractions, nasal flaring).
- Work of Breathing: Is Richard exhibiting signs of increased effort in breathing? Look for grunting, nasal flaring, use of accessory muscles, or paradoxical chest wall movement (a sign of respiratory distress).
- Oxygen Saturation (SpO2): Observe the pulse oximetry reading. A consistently low SpO2 indicates hypoxemia, requiring immediate attention. Note any fluctuations or trends in SpO2 readings.
- Color: Assess skin color for cyanosis (bluish discoloration), which suggests hypoxia. Observe for pallor, which can indicate anemia or other underlying issues affecting oxygenation.
- Level of Consciousness: Changes in alertness or responsiveness can be subtle indicators of worsening respiratory status or hypoxia.
- Positioning: Note Richard's posture. Patients in respiratory distress often adopt a tripod position (leaning forward with hands on knees or a surface) to facilitate breathing.
2. Auscultation: Listening to the Lungs
Auscultation is paramount in respiratory assessments. Using the virtual stethoscope in Shadow Health, systematically listen to lung sounds in all lung fields:
- Breath Sounds: Identify normal breath sounds (vesicular, bronchovesicular, bronchial). Note any adventitious sounds like crackles (fine or coarse), wheezes (high-pitched or low-pitched), rhonchi (low-pitched, snorous sounds), or pleural rubs (grating sounds). Document the location and characteristics of each abnormal sound. Remember the anatomical locations of lung fields.
- Lung Sounds: Interpretation and Significance:
- Crackles: Often indicate fluid in the airways or alveoli (pneumonia, pulmonary edema).
- Wheezes: Suggest airway narrowing (asthma, bronchitis).
- Rhonchi: Indicate secretions in larger airways (bronchitis, pneumonia).
- Absent Breath Sounds: May suggest atelectasis (collapsed lung), pneumothorax (collapsed lung), or pleural effusion (fluid in the pleural space).
- Technique: Use the diaphragm of the stethoscope and listen carefully, comparing sounds bilaterally.
3. Palpation: Feeling for Subtleties
Palpation complements auscultation. Lightly palpate the chest wall to assess:
- Chest Expansion: Assess symmetry of chest expansion during inspiration. Unequal expansion may indicate underlying lung pathology or pleural effusion.
- Tactile Fremitus: Feel for vibrations transmitted through the chest wall during speech. Increased fremitus suggests consolidation (e.g., pneumonia), while decreased fremitus may indicate air trapping (e.g., pneumothorax or emphysema).
4. Percussion: Tapping for Density
Percussion helps assess the density of underlying lung tissue:
- Technique: Using the middle finger of one hand, tap gently on the intercostal spaces. Listen for the resonance of the sounds.
- Interpretation: Dullness on percussion suggests consolidation (e.g., pneumonia, pleural effusion), while hyperresonance suggests increased air trapping (e.g., pneumothorax or emphysema).
5. Subjective Data: The Patient's Perspective
Engaging Richard in conversation is crucial:
- Symptoms: Inquire about his current symptoms (cough, shortness of breath, chest pain, sputum production, fever, chills). Use open-ended questions to elicit detailed descriptions. Ask about the onset, character, severity, and duration of symptoms.
- Past Medical History: Understanding his past medical history, including previous respiratory illnesses, surgeries, or allergies, is vital.
- Medications: Review the medications Richard is taking, paying close attention to respiratory medications (bronchodilators, corticosteroids, antibiotics).
- Allergies: Document any known allergies, particularly to medications.
- Current Treatment: Assess the effectiveness of current therapies. Inquire about any side effects.
- Pain: Thoroughly assess pain level using a scale (e.g., 0-10 scale) and describe the pain's location, character, and radiation.
Interpreting Findings and Developing a Plan
After a complete assessment, synthesize your findings. Identify any trends or patterns in Richard's condition. Based on your assessment, develop a care plan that addresses his immediate needs. This might involve:
- Increasing Oxygen Support: If SpO2 is low, adjust oxygen flow rate or consider alternative oxygen delivery methods (e.g., non-rebreather mask, high-flow nasal cannula).
- Administering Medications: If indicated, administer prescribed medications (e.g., bronchodilators, corticosteroids).
- Respiratory Treatments: Initiate or adjust respiratory treatments like nebulizer treatments or chest physiotherapy.
- Positioning: Adjust Richard's position to facilitate breathing (e.g., semi-Fowler's position, high-Fowler's position).
- Notification of Healthcare Provider: If Richard's condition is worsening rapidly, promptly notify the healthcare provider.
- Documentation: Meticulously document all observations, interventions, and responses to treatment.
Potential Pitfalls and Strategies for Success
- Inaccurate Auscultation: Practice proper stethoscope technique to avoid missing subtle lung sounds.
- Overlooking Subtle Changes: Pay meticulous attention to small changes in respiratory rate, rhythm, or oxygen saturation.
- Insufficient Questioning: Use open-ended and follow-up questions to gather comprehensive information.
- Poor Documentation: Ensure accurate and detailed documentation of all findings and interventions.
Conclusion: Mastering the Art of Respiratory Assessment
Performing hourly respiratory rounds on a patient like Richard in Shadow Health requires a combination of knowledge, skill, and attention to detail. By mastering the techniques outlined in this guide, you will improve your clinical judgment, enhance your ability to identify subtle changes in respiratory status, and ultimately provide safer and more effective patient care. Remember to practice regularly, reflecting on your findings and refining your assessment skills. Consistent practice with Shadow Health will translate into improved clinical competence. The ability to accurately assess and respond to respiratory changes is a cornerstone of safe and effective healthcare. This thorough approach will prepare you for real-world scenarios, enhancing your confidence and competence as a healthcare professional.
Latest Posts
Latest Posts
-
Esta Manana Comi Frutas En El
Mar 17, 2025
-
10 2 3 Select And Configure Dual Monitors
Mar 17, 2025
-
The Dutch Hunger Winter Case Study Answers
Mar 17, 2025
-
Journey To The Center Of The Earth Book Notes
Mar 17, 2025
-
No Man Is An Island Commonlit Answers
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about Respiratory System Hourly Rounds Shadow Health Richard . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
