Rn Adult Medical Surgical Myocardial Infarction Complications
Onlines
Mar 26, 2025 · 7 min read
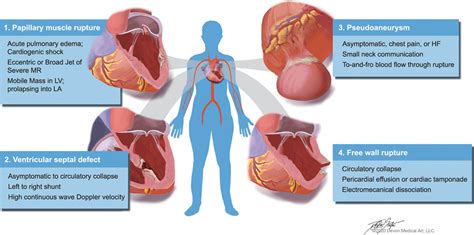
Table of Contents
RN Adult Medical Surgical: Myocardial Infarction Complications – A Comprehensive Guide
Myocardial infarction (MI), commonly known as a heart attack, occurs when blood flow to a part of the heart muscle is blocked. This blockage, usually caused by a blood clot in a coronary artery, deprives the heart muscle of oxygen, leading to cell death. While prompt treatment significantly improves outcomes, various complications can arise after an MI, demanding vigilant nursing care. This comprehensive guide explores these complications, focusing on the role of the Registered Nurse (RN) in adult medical-surgical settings.
Understanding the Pathophysiology of MI Complications
The severity and type of complications following an MI depend on several factors, including the extent of myocardial damage, the patient's pre-existing health conditions, and the effectiveness of treatment. The lack of oxygen to the heart muscle triggers a cascade of events, potentially leading to life-threatening consequences. These complications are often interconnected and can exacerbate each other.
1. Arrhythmias: The Most Common Threat
Arrhythmias, or abnormal heart rhythms, are the most frequent complication post-MI. The damaged heart muscle disrupts the electrical conduction system, leading to various arrhythmias, including:
- Ventricular tachycardia (VT): A rapid heart rhythm originating in the ventricles. This can be life-threatening and potentially lead to ventricular fibrillation.
- Ventricular fibrillation (VF): A chaotic, disorganized rhythm resulting in ineffective pumping of the heart. VF is a life-threatening emergency requiring immediate defibrillation.
- Atrial fibrillation (AF): An irregular heart rhythm originating in the atria. AF increases the risk of stroke due to the formation of blood clots.
- Bradycardia: A slow heart rate that can compromise cardiac output and lead to decreased tissue perfusion.
Nursing Implications: Continuous cardiac monitoring is crucial. The RN must be proficient in recognizing and responding to arrhythmias, initiating appropriate interventions as per protocols, including administering antiarrhythmic medications and preparing for cardioversion or defibrillation. Accurate documentation of rhythm changes and interventions is essential.
2. Cardiogenic Shock: A Life-Threatening Complication
Cardiogenic shock is a severe complication where the heart is unable to pump enough blood to meet the body's metabolic demands. This occurs when a significant portion of the heart muscle is damaged, resulting in a compromised ejection fraction. Symptoms include hypotension, tachycardia, cool and clammy skin, oliguria (decreased urine output), and altered mental status.
Nursing Implications: Management of cardiogenic shock requires aggressive interventions, including intravenous fluids, inotropes (medications that increase heart contractility), and possibly mechanical circulatory support devices like intra-aortic balloon pumps (IABP) or extracorporeal membrane oxygenation (ECMO). The RN plays a critical role in monitoring hemodynamic parameters, administering medications, and providing meticulous fluid balance management. Close collaboration with the cardiologist and other members of the healthcare team is essential.
3. Heart Failure: A Gradual Deterioration
Heart failure (HF) develops when the heart muscle is weakened and unable to pump efficiently. Post-MI, HF can be a delayed complication, as the damaged heart muscle struggles to maintain adequate cardiac output over time. Symptoms include shortness of breath, fatigue, edema (swelling), and persistent cough.
Nursing Implications: The RN focuses on managing symptoms, administering medications (diuretics, ACE inhibitors, beta-blockers), monitoring fluid status, and educating the patient on lifestyle modifications, including diet and activity restrictions. Regular assessment of respiratory status, weight, and fluid intake/output is vital.
4. Pericarditis: Inflammation of the Pericardium
Pericarditis, inflammation of the sac surrounding the heart (pericardium), can occur after an MI. This inflammation can lead to pericardial effusion (fluid accumulation in the pericardial sac) and cardiac tamponade (compression of the heart by the accumulated fluid), a life-threatening condition.
Nursing Implications: The RN assesses for symptoms like chest pain (often described as sharp and pleuritic), friction rub (auscultated on cardiac examination), and shortness of breath. Monitoring vital signs and cardiac rhythm is crucial. Treatment might involve pericardiocentesis (removal of fluid from the pericardial sac) or medications to reduce inflammation.
5. Papillary Muscle Dysfunction or Rupture: Valve Complications
The papillary muscles, responsible for opening and closing the mitral and tricuspid valves, can be damaged during an MI. Dysfunction or rupture of these muscles can lead to mitral regurgitation (leakage of blood back into the left atrium) or tricuspid regurgitation, compromising cardiac output.
Nursing Implications: Assessment for symptoms of heart failure, such as shortness of breath and edema, is crucial. Auscultation of heart sounds may reveal murmurs indicative of valvular regurgitation. Echocardiography is used to confirm the diagnosis. Management focuses on supporting cardiac function and possibly surgical intervention.
6. Ventricular Aneurysm: Weakening of the Ventricular Wall
A ventricular aneurysm is a bulging or weakened area of the ventricular wall, which can develop weeks or months after an MI. This weakened area can be a source of arrhythmias and thrombus formation, leading to stroke or other embolic events.
Nursing Implications: Regular monitoring for signs and symptoms of heart failure, arrhythmias, and embolic events is essential. The RN plays a crucial role in educating the patient about the importance of adherence to prescribed medication and lifestyle modifications to minimize complications.
7. Pulmonary Edema: Fluid Buildup in the Lungs
Pulmonary edema, the accumulation of fluid in the lungs' air sacs, can occur as a complication of an MI, especially in the context of left ventricular failure. It's characterized by shortness of breath, coughing (often with frothy sputum), and crackles heard on lung auscultation.
Nursing Implications: The RN needs to provide supportive care, including oxygen therapy, monitoring respiratory status closely, and managing fluid balance. Administration of diuretics may be necessary to reduce fluid overload. Positioning the patient upright may help alleviate respiratory distress.
8. Dressler's Syndrome: Post-MI Pericarditis and Pleuritis
Dressler's syndrome is a rare but potentially serious complication characterized by pericarditis and pleuritis (inflammation of the lining of the lungs) that occurs several weeks after an MI. It is believed to be an autoimmune reaction to the damaged heart muscle.
Nursing Implications: The RN needs to carefully monitor the patient for symptoms such as chest pain, fever, and shortness of breath. Treatment usually involves anti-inflammatory medications.
The RN's Role in Managing MI Complications
The RN plays a vital role in the prevention, early detection, and management of MI complications. This involves:
- Continuous cardiac monitoring: Closely observing the ECG for any rhythm disturbances.
- Hemodynamic monitoring: Regularly monitoring blood pressure, heart rate, and oxygen saturation.
- Assessment of respiratory status: Listening to lung sounds, assessing respiratory rate and effort.
- Fluid balance monitoring: Measuring intake and output, assessing for signs of fluid overload or dehydration.
- Medication administration: Administering medications as ordered, including antiarrhythmics, inotropes, diuretics, anticoagulants, and analgesics.
- Patient education: Teaching patients about their condition, medications, lifestyle modifications, and the importance of adherence to the treatment plan.
- Early recognition of complications: Promptly identifying and reporting any signs or symptoms of potential complications.
- Collaboration with the healthcare team: Working closely with the physician, cardiologist, respiratory therapist, and other healthcare professionals.
Preventing MI Complications: A Proactive Approach
Prevention is key in minimizing the risk of MI complications. Strategies include:
- Early recognition and treatment of MI: Prompt reperfusion therapy (e.g., thrombolysis or PCI) minimizes myocardial damage.
- Aggressive risk factor modification: Managing hypertension, hyperlipidemia, diabetes, and smoking cessation.
- Appropriate medication management: Using beta-blockers, ACE inhibitors, and antiplatelet agents to prevent recurrent events.
- Cardiac rehabilitation: Engaging in a supervised exercise program and lifestyle modifications.
Conclusion: A Collaborative Effort for Optimal Outcomes
Managing MI complications requires a multifaceted approach. The RN's expertise in assessment, medication administration, and patient education is crucial in optimizing patient outcomes. A collaborative effort involving the entire healthcare team, focusing on early detection, prompt intervention, and diligent patient monitoring, significantly improves the chances of a positive recovery and reduces the risk of mortality. Staying abreast of the latest advancements in MI management, including evolving treatment protocols and technological innovations, is vital for RNs in this specialized area of care. By consistently applying evidence-based practices and maintaining a patient-centered approach, RNs play a pivotal role in enhancing the quality of life for individuals recovering from myocardial infarction.
Latest Posts
Latest Posts
-
A Patients Son Calls To Ask For Information
Mar 29, 2025
-
Characters In Do Androids Dream Of Electric Sheep
Mar 29, 2025
-
A Small Compact Car Was Involved In A Rollover Crash
Mar 29, 2025
-
Sick Call At Detention Facilities Must Be Held
Mar 29, 2025
-
Lewis Med Surg 12th Edition Test Bank
Mar 29, 2025
Related Post
Thank you for visiting our website which covers about Rn Adult Medical Surgical Myocardial Infarction Complications . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
