Select The True Statements Regarding Blood Type
Onlines
Mar 20, 2025 · 7 min read
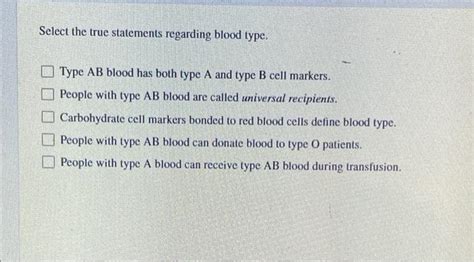
Table of Contents
Select the True Statements Regarding Blood Type: A Comprehensive Guide
Understanding blood types is crucial in various aspects of healthcare, from blood transfusions to pregnancy. The seemingly simple A, B, AB, and O system hides a fascinating complexity, and misconceptions abound. This comprehensive guide will delve into the intricacies of blood typing, clarifying common misunderstandings and highlighting key facts. We'll explore the science behind blood groups, their inheritance patterns, and their clinical significance.
The ABO Blood Group System: The Basics
The ABO system, the most important blood group system, categorizes blood into four primary types: A, B, AB, and O. These designations refer to the presence or absence of specific antigens – substances that can trigger an immune response – on the surface of red blood cells (erythrocytes).
- Type A blood: Possesses A antigens on red blood cells and anti-B antibodies in the plasma.
- Type B blood: Possesses B antigens on red blood cells and anti-A antibodies in the plasma.
- Type AB blood: Possesses both A and B antigens on red blood cells and neither anti-A nor anti-B antibodies in the plasma.
- Type O blood: Possesses neither A nor B antigens on red blood cells and both anti-A and anti-B antibodies in the plasma.
This seemingly simple system has profound implications for blood transfusions. Incompatible transfusions, where the recipient's antibodies react against the donor's antigens, can lead to a life-threatening reaction. This is why blood type matching is critical before any blood transfusion.
True Statements Regarding ABO Blood Types:
-
Blood type is inherited: Your blood type is determined by the genes you inherit from your parents. Each parent contributes one allele (gene variant) for the ABO blood group system. The combination of these alleles determines your blood type. This inheritance pattern follows Mendelian genetics.
-
Antibodies are naturally occurring: The antibodies in your plasma are not produced in response to exposure to foreign blood; they are naturally present. This means individuals with type A blood have anti-B antibodies, even without prior exposure to type B blood. Similarly, individuals with type B blood have anti-A antibodies.
-
Type O is the universal donor (for red blood cells): Since type O blood lacks A and B antigens, it can be transfused to individuals of all ABO blood types in emergency situations. However, it's crucial to note that this only applies to red blood cells. Other blood components, like plasma, might still cause reactions.
-
Type AB is the universal recipient (for red blood cells): Because individuals with type AB blood lack anti-A and anti-B antibodies, they can theoretically receive red blood cells from all ABO blood types. Again, this only pertains to red blood cells. Plasma compatibility remains a consideration.
-
Blood type is clinically significant: Blood type is a critical factor in blood transfusions, organ transplants, and even during pregnancy (Rh factor compatibility is also crucial in pregnancy). Mismatched blood transfusions can result in severe complications, including hemolysis (destruction of red blood cells), kidney failure, and even death.
Beyond ABO: The Rh Factor and Other Blood Group Systems
While the ABO system is the most well-known, it's only one of many blood group systems. The Rh factor is another crucial system, adding further complexity to blood type categorization.
The Rh factor is a protein found on the surface of red blood cells. Individuals who possess this protein are considered Rh-positive (Rh+), while those who lack it are Rh-negative (Rh-). This adds another layer to blood typing, resulting in eight common blood types: A+, A-, B+, B-, AB+, AB-, O+, and O-.
True Statements Regarding the Rh Factor:
-
Rh incompatibility can cause hemolytic disease of the newborn (HDN): If an Rh-negative mother carries an Rh-positive fetus, there's a risk of HDN. During pregnancy or delivery, the mother may develop antibodies against the fetal Rh-positive blood. In subsequent pregnancies with Rh-positive fetuses, these antibodies can cross the placenta and attack the fetal red blood cells, leading to anemia and other complications. This risk is mitigated by administering RhoGAM to Rh-negative mothers.
-
Rh factor is inherited independently of ABO: The Rh factor and ABO blood group are inherited separately. A person can have any combination of ABO and Rh types.
-
Rh-negative individuals do not naturally possess anti-Rh antibodies: Unlike the ABO system, Rh-negative individuals do not naturally possess anti-Rh antibodies. These antibodies only develop after exposure to Rh-positive blood, typically through pregnancy or a blood transfusion.
Other Blood Group Systems: A Glimpse into Complexity
Beyond ABO and Rh, numerous other blood group systems exist, each with its own set of antigens and antibodies. These include:
- Duffy system: Plays a role in malaria susceptibility.
- Kell system: Important in blood transfusions and HDN.
- MNS system: Less clinically significant than ABO and Rh.
- Lewis system: Often found in saliva and other body fluids.
- Lutheran system: Relatively rare antigens.
These systems, although less frequently discussed, are nonetheless important in ensuring safe blood transfusions and understanding various medical conditions. The presence or absence of antigens within these systems can lead to further complexities in blood compatibility.
Implications for Blood Transfusions and Organ Transplantation
Understanding the intricacies of blood types is paramount in the field of transfusion medicine. The principles of compatibility are crucial to prevent adverse reactions.
True Statements Regarding Blood Transfusions and Organ Transplantation:
-
Careful matching is essential: Before a blood transfusion, rigorous testing is performed to ensure compatibility between the donor and recipient's blood types. This includes ABO and Rh matching, as well as cross-matching, where a small sample of the donor's blood is mixed with the recipient's serum to check for any agglutination (clumping) reactions.
-
Incompatible transfusions can be life-threatening: Transfusing incompatible blood can lead to a severe transfusion reaction, characterized by fever, chills, hypotension, and potentially organ damage or death.
-
Organ transplantation also requires blood type consideration: While not as strictly limited as blood transfusions, organ transplantation also considers blood type compatibility. A closer match between donor and recipient blood types generally leads to better graft survival rates.
-
Blood type compatibility affects pregnancy: As mentioned earlier, Rh incompatibility can cause HDN. Careful monitoring and preventative measures are necessary in pregnancies involving Rh-incompatible mothers and fetuses.
-
Rare blood types require specialized care: Individuals with rare blood types, whether due to ABO, Rh, or other blood group systems, require specialized care in case of emergencies, as finding compatible donors can be challenging.
Dispelling Myths and Misconceptions
Numerous misconceptions surround blood types. It's important to address these to ensure a clear understanding:
-
Blood type personality tests are not scientifically valid: Claims linking blood type to personality traits lack scientific backing and are considered pseudoscience.
-
Diet based on blood type has no proven effectiveness: The idea that diet should be tailored to blood type has not been supported by rigorous scientific evidence.
-
Blood type alone doesn't determine overall health: While blood type is relevant in certain medical contexts, it's not a predictor of general health or susceptibility to specific diseases.
Conclusion: The Ever-Evolving Understanding of Blood Groups
The study of blood groups is a dynamic field, with ongoing research uncovering new antigens and systems. This complex interplay of antigens and antibodies highlights the importance of thorough blood typing and cross-matching procedures before any blood transfusion or organ transplantation. Accurate knowledge about blood types is essential not only for healthcare professionals but also for individuals to understand their own health and make informed decisions. The seemingly simple categorization of A, B, AB, and O belies a much richer, more intricate reality with far-reaching implications for health and medicine. Continued research promises further advancements in our understanding of these vital biological markers, improving healthcare outcomes worldwide.
Latest Posts
Latest Posts
-
Relational Issues Are Inextricably Bound To Content Issues
Mar 20, 2025
-
Trust The Skinny Chef Cookbook Pdf
Mar 20, 2025
-
Green Leaf By Flannery O Connor Summerize Short
Mar 20, 2025
-
Experiment 34 An Equilibrium Constant Lab Report
Mar 20, 2025
-
All Music Has A Strong Discernable Beat
Mar 20, 2025
Related Post
Thank you for visiting our website which covers about Select The True Statements Regarding Blood Type . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
