Shadow Health Uti With Antibiotic Sensitivity Medication Selection
Onlines
Mar 17, 2025 · 6 min read
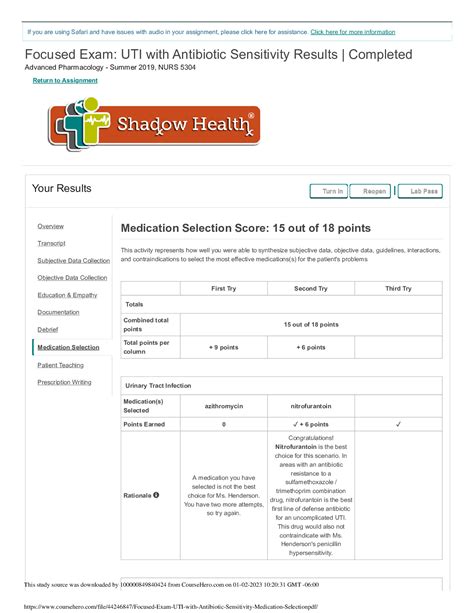
Table of Contents
Shadow Health UTI with Antibiotic Sensitivity: Medication Selection and Patient Management
The accurate diagnosis and treatment of urinary tract infections (UTIs) are crucial for patient well-being. This article delves into the virtual UTI patient simulation offered by Shadow Health, focusing on the critical process of antibiotic sensitivity testing and subsequent medication selection. We'll explore the clinical reasoning behind choosing the appropriate antibiotic, emphasizing the importance of considering patient factors and potential adverse effects. Understanding these aspects is paramount for effective UTI management, minimizing the risk of treatment failure and the development of antibiotic resistance.
Understanding Urinary Tract Infections (UTIs)
UTIs are among the most common bacterial infections, affecting both men and women, though women are significantly more susceptible. These infections can range from uncomplicated cystitis (bladder infection) to more severe pyelonephritis (kidney infection). Symptoms vary depending on the location and severity of the infection but commonly include:
- Dysuria: Painful or burning urination
- Frequency: Increased urinary frequency
- Urgency: Sudden, strong urge to urinate
- Suprapubic pain: Pain or discomfort above the pubic bone (bladder area)
- Hematuria: Blood in the urine (may or may not be visible)
- Fever and chills: Often indicative of more severe infections like pyelonephritis
- Flank pain: Pain in the side/back, suggesting kidney involvement
Diagnostic Approach in Shadow Health UTI Simulation
The Shadow Health UTI simulation provides a virtual patient encounter mirroring real-world clinical scenarios. The diagnostic process typically involves:
- Patient history: Gathering a comprehensive medical history, including symptoms, duration of symptoms, past medical history, and allergies. This is crucial for identifying risk factors and potential contraindications to certain medications.
- Physical examination: Performing a virtual physical examination to assess vital signs (temperature, blood pressure, heart rate, respiratory rate) and identify any physical signs of infection.
- Urinalysis: Interpreting urinalysis results, including leukocyte esterase, nitrites, and microscopic examination for bacteria, white blood cells, and red blood cells. These tests help confirm the presence of a UTI and provide initial clues about the severity.
- Urine culture and sensitivity (C&S): This is the cornerstone of appropriate antibiotic selection. The urine culture identifies the specific bacteria causing the infection, while the sensitivity testing determines which antibiotics are effective against that particular strain. This is crucial for targeted therapy and minimizing the risk of antibiotic resistance.
The Importance of Antibiotic Sensitivity Testing
The rise of antibiotic-resistant bacteria represents a major global health threat. Empiric antibiotic therapy (treatment before culture results are available) can be necessary in severe cases, but ideally, treatment should be guided by the results of the urine culture and sensitivity test. This approach ensures that the chosen antibiotic will effectively eliminate the infecting organism while minimizing the risk of developing resistance.
Interpreting Sensitivity Results
Antibiotic sensitivity reports often use terms like:
- Susceptible (S): The bacteria are inhibited by the antibiotic at clinically achievable concentrations. This indicates the antibiotic is a good treatment option.
- Intermediate (I): The bacteria's growth is inhibited by the antibiotic at higher concentrations than typically achievable. This may be a treatment option if higher doses are considered, but other susceptible antibiotics are often preferred.
- Resistant (R): The bacteria are not inhibited by the antibiotic at clinically achievable concentrations. This antibiotic is not a suitable treatment option.
The report will list numerous antibiotics with their corresponding susceptibility designation (S, I, or R). This information guides the physician in selecting the most appropriate and effective antibiotic.
Antibiotic Selection for UTIs in Shadow Health
The choice of antibiotic in the Shadow Health UTI simulation, as in real-world practice, depends on several factors:
- Identification of the infecting organism: Gram-positive or Gram-negative bacteria. Different antibiotics are effective against different types of bacteria. Escherichia coli (E. coli) is the most common cause of UTIs, followed by Staphylococcus saprophyticus, Klebsiella pneumoniae, and Proteus mirabilis.
- Antibiotic susceptibility profile: The results from the urine culture and sensitivity test are crucial. Choose an antibiotic to which the isolated bacteria is susceptible.
- Patient factors: Age, pregnancy, allergies, renal function, and other comorbidities influence antibiotic selection. Some antibiotics are contraindicated in certain populations (e.g., tetracyclines in pregnancy, fluoroquinolones in children and the elderly).
- Potential adverse effects: All antibiotics have the potential for side effects. Consider the patient’s overall health and risk factors when assessing the risk-benefit ratio of different antibiotics. Common side effects include gastrointestinal upset (nausea, vomiting, diarrhea), allergic reactions, and changes in the normal gut flora.
- Drug interactions: Check for any potential drug interactions between the chosen antibiotic and other medications the patient is currently taking.
- Treatment duration: The duration of antibiotic therapy depends on the severity of the infection and the patient's response to treatment. Typically, uncomplicated UTIs are treated for 3-7 days.
Examples of Common Antibiotics Used for UTIs
Several antibiotics are commonly used to treat UTIs, including:
- Nitrofurantoin: Often a first-line choice for uncomplicated UTIs caused by susceptible organisms. However, it is not effective against many Gram-negative bacteria and is not suitable for patients with impaired renal function.
- Trimethoprim-sulfamethoxazole (TMP-SMX): Another common first-line choice, but resistance is increasing in some regions. It's contraindicated in patients with sulfa allergies.
- Fosfomycin: A single-dose treatment option for uncomplicated UTIs, suitable for patients who cannot tolerate multiple days of therapy.
- Fluoroquinolones (e.g., ciprofloxacin, levofloxacin): Generally reserved for more complicated UTIs or when other antibiotics have failed. Their use is increasingly restricted due to the potential for serious side effects and the development of resistance.
- Cephalosporins (e.g., cefixime, cefpodoxime): May be used as alternatives to other first-line agents, particularly in cases of TMP-SMX resistance.
- Beta-lactam antibiotics (e.g., Amoxicillin): Less commonly used for UTIs as resistance is common but might be considered when sensitivity testing shows its efficacy.
Managing UTI Patients: Beyond Antibiotic Selection
Effective UTI management goes beyond simply prescribing antibiotics. It encompasses patient education and monitoring:
- Patient education: Explain the infection, its treatment, and the importance of completing the entire course of antibiotics. Instruct the patient on recognizing and reporting any side effects. Emphasize the importance of adequate hydration.
- Follow-up: Schedule a follow-up appointment to assess the patient's response to treatment and to monitor for any complications. A repeat urine culture may be necessary to confirm eradication of the infection.
- Prevention: Discuss preventive strategies, such as drinking plenty of fluids, urinating frequently, and practicing good hygiene. For recurrent UTIs, prophylactic antibiotics may be considered but should be used cautiously to minimize resistance development.
Addressing Potential Complications
In some cases, UTIs can lead to complications such as:
- Pyelonephritis: Kidney infection, requiring hospitalization and intravenous antibiotics.
- Sepsis: A life-threatening bloodstream infection.
- Urosepsis: Sepsis caused by a UTI.
- Renal abscess: Localized collection of pus in the kidney.
Prompt diagnosis and treatment are vital to prevent these severe complications. The Shadow Health simulation provides opportunities to practice identifying and managing such scenarios.
Conclusion
The Shadow Health UTI simulation offers a valuable platform to practice the crucial steps involved in diagnosing and managing UTIs. By correctly interpreting urinalysis, culture and sensitivity results, and carefully considering patient-specific factors, clinicians can select the most appropriate antibiotic and ensure optimal patient outcomes. Remembering that antibiotic stewardship is critical; appropriate antibiotic selection minimizes the risk of treatment failure and the development of antibiotic-resistant bacteria. Effective communication with the patient and timely follow-up are equally vital aspects of successful UTI management. Mastering these elements is paramount for providing high-quality care and promoting patient well-being.
Latest Posts
Latest Posts
-
Coral Bleaching Can Be Hazardous To Some Fish Species Because
Mar 17, 2025
-
Sleep Awareness Week Begins In The Spring With The Release
Mar 17, 2025
-
Select The Correct Answer From Each Drop Down Menu
Mar 17, 2025
-
Christian High School Equivalency Exam Answers
Mar 17, 2025
-
Introduction To Health Assessment 3 0 Test
Mar 17, 2025
Related Post
Thank you for visiting our website which covers about Shadow Health Uti With Antibiotic Sensitivity Medication Selection . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
