Skills Module 3.0: Closed-chest Drainage Posttest
Onlines
Mar 28, 2025 · 6 min read
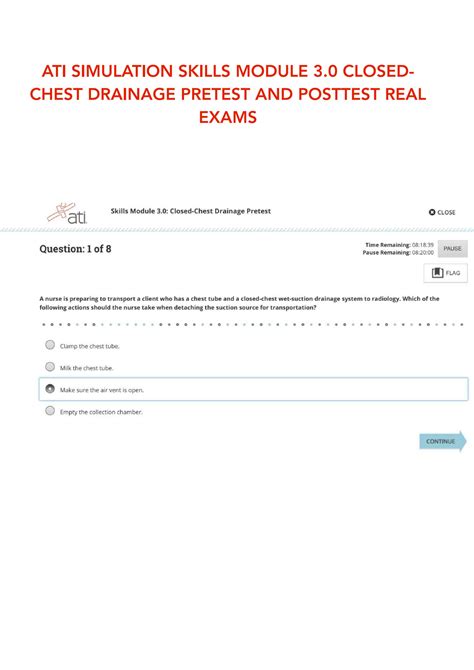
Table of Contents
Skills Module 3.0: Closed-Chest Drainage Post-Test - A Comprehensive Guide
This comprehensive guide delves into the intricacies of a Skills Module 3.0 post-test focused on closed-chest drainage (CCD), equipping you with the knowledge and understanding needed to excel. We'll cover key concepts, crucial assessment points, potential complications, and strategies for effective learning and test preparation. This in-depth analysis goes beyond simple question-answer scenarios, providing a holistic understanding of CCD management.
Understanding Closed-Chest Drainage (CCD)
Closed-chest drainage (also known as chest tube drainage) is a vital procedure used to remove air or fluid from the pleural space, the area between the lungs and the chest wall. This space should normally be under negative pressure to allow for proper lung expansion. Accumulation of air (pneumothorax) or fluid (hemothorax, pleural effusion) can compromise lung function, leading to respiratory distress and even life-threatening complications. CCD systems provide a pathway for this air or fluid to be evacuated, restoring negative pressure and allowing the lung to re-expand.
Key Components of a Closed-Chest Drainage System:
- Chest Tube: A flexible tube inserted through the chest wall into the pleural space.
- Collection Chamber: A container that collects the drained fluid and air. This chamber often has markings to measure drainage volume.
- Water Seal Chamber: This crucial component prevents air from re-entering the pleural space while allowing air and fluid to exit. The characteristic bubbling in this chamber is a normal finding, indicating that air is escaping the pleural space.
- Suction Control Chamber (Optional): Some systems incorporate a suction control chamber to regulate the amount of suction applied to the pleural space. This is often adjustable.
Skills Module 3.0 Post-Test: Expected Knowledge and Application
The Skills Module 3.0 post-test on closed-chest drainage will likely assess your understanding and practical application of various aspects of CCD management. Expect questions and scenarios covering the following areas:
1. Indications for Closed-Chest Drainage:
- Pneumothorax: Collapsed lung due to air in the pleural space. This can be spontaneous, traumatic, or tension pneumothorax (a life-threatening condition).
- Hemothorax: Blood in the pleural space, often resulting from trauma or surgery.
- Pleural Effusion: Fluid accumulation in the pleural space due to various causes, including infection, heart failure, or cancer.
- Empyema: Pus in the pleural space, indicating infection.
2. Pre-Procedure Assessment and Preparation:
- Patient History: Gathering information about the patient's medical history, including underlying conditions and the cause of the pleural effusion or pneumothorax.
- Physical Examination: Assessing respiratory status, including breath sounds, respiratory rate, and oxygen saturation. Inspecting the chest for any signs of trauma or distress.
- Imaging Studies: Reviewing chest X-rays or CT scans to confirm the diagnosis and guide tube placement.
3. Procedure: Insertion and Maintenance of Chest Tube:
- Aseptic Technique: Strict adherence to sterile procedures to prevent infection.
- Tube Placement: Understanding the anatomical landmarks and appropriate insertion sites.
- Securing the Tube: Proper techniques for anchoring the chest tube to prevent dislodgement.
- Connecting the Drainage System: Correctly connecting the chest tube to the collection chamber and water seal chamber.
4. Post-Procedure Care and Monitoring:
- Drainage Monitoring: Regularly assessing the amount and character of drainage.
- Tube Patency: Ensuring the chest tube remains patent (unblocked).
- Water Seal Chamber Observation: Monitoring for bubbling and tidaling (fluctuation of the water level with respiration). Understanding what constitutes normal and abnormal findings.
- Patient Assessment: Continuously monitoring vital signs, respiratory status, and pain levels.
- Potential Complications: Recognizing and responding to potential complications, such as tube dislodgement, air leaks, and infection.
5. Troubleshooting: Identifying and Addressing Potential Issues:
- Air Leaks: Identifying the source of an air leak and taking appropriate actions.
- Clots in the Drainage System: Managing clots and maintaining tube patency.
- Tube Kinking or Obstruction: Addressing kinks or obstructions in the drainage system.
- Accidental Removal of the Tube: Immediate management of accidental tube removal.
6. Documentation: Accurate and Thorough Record Keeping:
- Drainage Volumes: Accurately documenting the amount of drainage at regular intervals.
- Patient Status: Recording vital signs, respiratory status, and any observed complications.
- Interventions: Documenting any interventions performed, such as suction adjustment or troubleshooting measures.
Strategies for Success on Your Post-Test
Thorough preparation is key to succeeding in your Skills Module 3.0 post-test. Here’s a multi-pronged approach:
1. Comprehensive Review of Course Material:
- Textbook and Lecture Notes: Revisit all relevant course materials, focusing on key concepts and procedures.
- Practice Questions: Work through practice questions and scenarios to reinforce your understanding and identify areas needing further review. Focus on applying your knowledge to realistic clinical situations.
2. Hands-on Practice and Simulation:
- Skills Labs: If possible, participate in skills labs or simulations to gain practical experience with chest tube insertion, maintenance, and troubleshooting. This hands-on experience is invaluable.
3. Collaborative Learning:
- Study Groups: Form a study group with peers to discuss challenging concepts, practice questions, and share knowledge. Explaining concepts to others strengthens your understanding.
4. Focus on High-Yield Areas:
- Prioritize Key Concepts: Concentrate your study efforts on high-yield areas, such as indications for CCD, complications, and post-procedure monitoring. Identify areas where you feel less confident and dedicate extra time to them.
5. Understanding the Rationale Behind Procedures:
- Why and How: Don't just memorize facts; understand the underlying rationale for each step of the procedure and the potential consequences of errors. This deeper understanding will help you answer complex questions.
6. Visualization and Mental Rehearsal:
- Picture the Scenario: Visualize the process of chest tube insertion, maintenance, and troubleshooting. Mentally rehearse the steps involved in managing various complications.
7. Time Management and Test-Taking Strategies:
- Practice Tests: Take practice tests under timed conditions to simulate the actual post-test environment. This will help you manage your time effectively and improve your test-taking strategies.
- Review Your Mistakes: Analyze your mistakes on practice tests to identify areas needing further review. Don't just focus on the correct answers; learn from your errors.
Addressing Potential Post-Test Questions
The following are examples of potential questions you might encounter on your Skills Module 3.0 post-test on closed-chest drainage. These examples are designed to illustrate the types of questions and the depth of understanding required. Remember, your specific post-test will vary.
Scenario-Based Questions:
- A patient with a chest tube suddenly experiences increased bubbling in the water seal chamber. What are the possible causes, and how would you assess and manage this situation?
- A patient with a chest tube reports sudden, sharp chest pain. What steps would you take to assess the patient and address the potential problem?
- You notice a significant decrease in chest tube drainage in a patient who was previously draining large volumes. What are some potential explanations, and how would you investigate this?
Knowledge-Based Questions:
- What are the key components of a closed-chest drainage system, and what is the function of each component?
- Describe the proper technique for assessing the patency of a chest tube.
- List three potential complications of closed-chest drainage and describe their management.
- Explain the difference between a pneumothorax and a hemothorax. What are the key clinical manifestations of each?
- Detail the indications for closed-chest drainage.
Critical Thinking Questions:
- A patient with a chest tube has continuous, vigorous bubbling in the water seal chamber. What does this indicate, and what is the priority nursing action?
- How would you educate a patient and their family about the purpose and care of a chest tube?
- You observe tidaling in the water seal chamber. Explain what this means and its significance.
This detailed guide provides a strong foundation for preparing for your Skills Module 3.0 post-test on closed-chest drainage. Remember that consistent study, hands-on practice, and a comprehensive understanding of the underlying principles are essential for success. Good luck!
Latest Posts
Latest Posts
-
Which Of The Following Does Not Distinguish A Blog
Mar 31, 2025
-
Of Mice And Men Chapter Synopsis
Mar 31, 2025
-
Lab 6 Saturation And Atmospheric Stability Answers
Mar 31, 2025
-
How Do Chloroplasts Capture Energy From The Sun Worksheet Answers
Mar 31, 2025
-
Summary Of Sundiata An Epic Of Old Mali
Mar 31, 2025
Related Post
Thank you for visiting our website which covers about Skills Module 3.0: Closed-chest Drainage Posttest . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
