Tina Jones Comprehensive Assessment Shadow Health
Onlines
Mar 03, 2025 · 7 min read
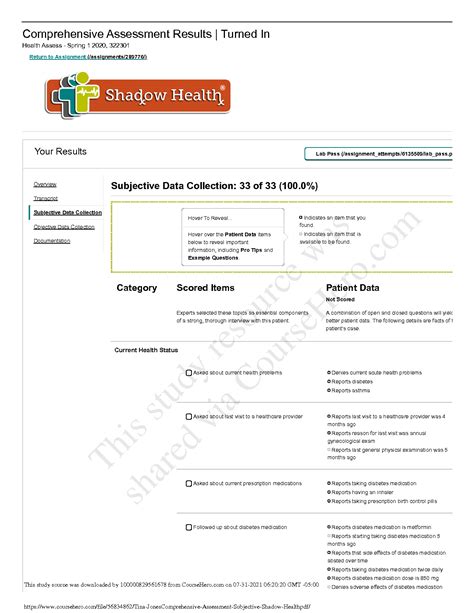
Table of Contents
Tina Jones Comprehensive Assessment: A Deep Dive into Shadow Health
Shadow Health's Tina Jones comprehensive assessment provides nursing students with an invaluable opportunity to practice their assessment skills in a risk-free virtual environment. This detailed exploration will guide you through each stage of the assessment, highlighting key findings, potential diagnoses, and crucial nursing interventions. We will delve into the subjective and objective data, analyze the patient's history, and discuss the rationale behind various diagnostic and treatment considerations. Mastering this comprehensive assessment is a cornerstone of successful nursing practice.
Understanding the Shadow Health Tina Jones Simulation
The Tina Jones simulation within Shadow Health is designed to mimic a real-world patient encounter. It's not just about memorizing facts; it's about applying nursing knowledge, critical thinking, and clinical judgment to develop a comprehensive care plan. The simulation allows for multiple attempts, encouraging iterative learning and refinement of assessment techniques. This iterative process helps solidify understanding of complex concepts and builds confidence in approaching diverse patient scenarios.
Subjective Data Collection: Listening to Tina Jones' Story
The subjective data collection phase focuses on what Tina Jones tells you. This information forms the foundation of your assessment and directs your subsequent objective findings. Key elements include:
Chief Complaint:
Tina Jones' chief complaint is usually centered around her presenting symptoms. Understanding the context and nature of her complaint is paramount. It sets the stage for the subsequent history-taking process. This isn't simply about recording her words; it's about understanding the impact of her symptoms on her daily life.
History of Present Illness (HPI):
This section requires a detailed exploration of the onset, character, location, duration, severity, timing, setting, associated factors, and relieving/aggravating factors of her symptoms. Effective HPI documentation demonstrates a thorough understanding of symptom analysis, a vital skill for any healthcare professional.
- Onset: When did the symptoms begin?
- Character: Describe the nature of the symptoms (e.g., sharp, dull, aching).
- Location: Where are the symptoms located?
- Duration: How long have the symptoms lasted?
- Severity: How intense are the symptoms (using a pain scale, for example)?
- Timing: When do the symptoms occur (e.g., morning, evening, continuously)?
- Setting: Where do the symptoms occur?
- Associated factors: Are there any other symptoms that occur alongside the primary complaint?
- Relieving/aggravating factors: What makes the symptoms better or worse?
Past Medical History (PMH):
This section encompasses Tina Jones' previous illnesses, surgeries, hospitalizations, and allergies. Understanding her medical history provides crucial context for her current condition. This information helps you anticipate potential complications and tailor your assessment and care plan accordingly.
Family History (FH):
Exploring Tina Jones' family history of illnesses, especially those with genetic predispositions, aids in identifying potential risk factors for her current and future health. It's essential to look for patterns and identify potential genetic influences.
Social History (SH):
This includes details about Tina Jones' lifestyle, including occupation, marital status, living situation, habits (smoking, alcohol, drug use), diet, exercise, and social support systems. This section paints a picture of her overall well-being and identifies potential environmental or lifestyle-related risk factors. Consider the impact of social determinants of health on her well-being.
Review of Systems (ROS):
The review of systems systematically explores each body system to identify any other symptoms that Tina Jones may not have spontaneously reported. It's a structured approach to ensure a comprehensive assessment, even if seemingly unrelated to the chief complaint. Each system should be thoroughly investigated, paying attention to any positive or negative findings.
Objective Data Collection: Performing the Physical Examination
This section focuses on the physical examination, where you systematically assess Tina Jones using your observation and examination skills.
General Appearance:
Begin by noting her overall appearance, including her level of consciousness, affect, respiratory effort, and skin color. These initial observations provide valuable clues about her overall health status.
Vital Signs:
Accurately measuring vital signs (temperature, pulse, respirations, blood pressure, and oxygen saturation) is essential. Any deviations from normal parameters require careful analysis and interpretation.
HEENT Examination:
A comprehensive HEENT (Head, Eyes, Ears, Nose, Throat) examination assesses the head, face, eyes, ears, nose, and throat. This involves inspecting for any abnormalities, including skin lesions, facial asymmetry, visual acuity, hearing deficits, nasal patency, and oral mucosal integrity.
Neck Examination:
Assess the neck for any abnormalities, including lymph node enlargement, thyroid gland enlargement, and jugular venous distention. Palpating the lymph nodes is crucial in identifying potential infections or other pathologies.
Cardiovascular Examination:
Auscultate the heart sounds for any murmurs, extra heart sounds, or arrhythmias. Palpate the carotid arteries for any bruits. This examination provides critical insights into cardiovascular health.
Respiratory Examination:
Auscultate the lungs for any adventitious breath sounds (wheezing, crackles, rhonchi). Percuss the lungs for resonance and assess respiratory effort. This is crucial for detecting respiratory conditions.
Abdominal Examination:
Perform a thorough abdominal examination, including inspection, auscultation, percussion, and palpation. Note any tenderness, distension, or masses. This assessment aids in identifying gastrointestinal problems.
Neurological Examination:
Assess mental status, cranial nerves, motor strength, sensory function, reflexes, and coordination. This is important for detecting neurological impairments.
Musculoskeletal Examination:
Examine joints for range of motion, tenderness, and swelling. Assess muscle strength and tone.
Skin Examination:
Assess the skin for lesions, rashes, temperature, turgor, and color. This identifies dermatological conditions and assesses hydration status.
Data Interpretation and Diagnostic Reasoning
After collecting both subjective and objective data, the next crucial step is interpretation. This involves analyzing the findings, identifying patterns, and formulating potential diagnoses. This stage requires strong clinical judgment and the ability to connect seemingly disparate pieces of information.
Differential Diagnoses: Based on the data gathered, formulate a list of potential diagnoses, ranging from the most likely to the least likely. Justify your reasoning for each diagnosis based on specific findings. This process demonstrates critical thinking and a systematic approach to problem-solving.
Prioritizing Diagnoses: Prioritize the diagnoses based on urgency and potential severity. Which conditions require immediate attention? Which can be addressed later? This prioritization is essential for effective care planning.
Developing a Nursing Care Plan
Once you've formulated potential diagnoses, it's time to develop a comprehensive nursing care plan. This plan should outline specific nursing interventions aimed at addressing the patient's needs and promoting optimal outcomes. A well-structured care plan should include:
- Nursing Diagnoses: Based on your assessment, formulate relevant nursing diagnoses using the NANDA-I framework.
- Expected Outcomes: Define measurable and achievable goals for each nursing diagnosis.
- Nursing Interventions: Outline specific actions you will take to achieve the desired outcomes.
- Evaluation: Describe how you will evaluate the effectiveness of your interventions.
Remember to tailor your nursing care plan to Tina Jones' individual needs and circumstances.
Reflective Practice: Learning from the Simulation
The Shadow Health Tina Jones simulation encourages reflective practice. After completing the assessment, take time to reflect on your performance. What went well? What could be improved? This self-assessment is crucial for continuous learning and professional development.
- Identify Strengths: Recognize areas where you performed effectively.
- Identify Weaknesses: Acknowledge areas where your performance could be improved.
- Develop Action Plan: Create a plan to address identified weaknesses.
- Seek Feedback: Discuss your performance with a preceptor or instructor for additional feedback.
Conclusion: Mastering the Tina Jones Assessment
The Tina Jones comprehensive assessment in Shadow Health is a powerful tool for nursing students. By mastering this simulation, you'll develop crucial skills in data collection, interpretation, diagnostic reasoning, and care planning. Remember, it’s a journey of continuous learning and refinement. Embrace the challenges, learn from your mistakes, and strive to become a confident and competent healthcare professional. The more you practice, the better you’ll become at identifying subtle cues and developing effective interventions for a wide range of patient scenarios. Remember that this detailed exploration only provides a framework; the nuances of each individual simulation will vary, adding to the richness and complexity of this learning experience.
Latest Posts
Latest Posts
-
Character Sketch Of Oliver In Oliver Twist
Mar 03, 2025
-
Cisco 1120 Disk Usage Frequent Drain Of Connection Events
Mar 03, 2025
-
To Kill A Mockingbird Summary Of Every Chapter
Mar 03, 2025
-
Song Charting Project Dear No One By Tori Kelly
Mar 03, 2025
-
The Director Of Health Services Is Concerned About A Possible
Mar 03, 2025
Related Post
Thank you for visiting our website which covers about Tina Jones Comprehensive Assessment Shadow Health . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
