Tina Jones Neurological Shadow Health Documentation
Onlines
Mar 23, 2025 · 6 min read
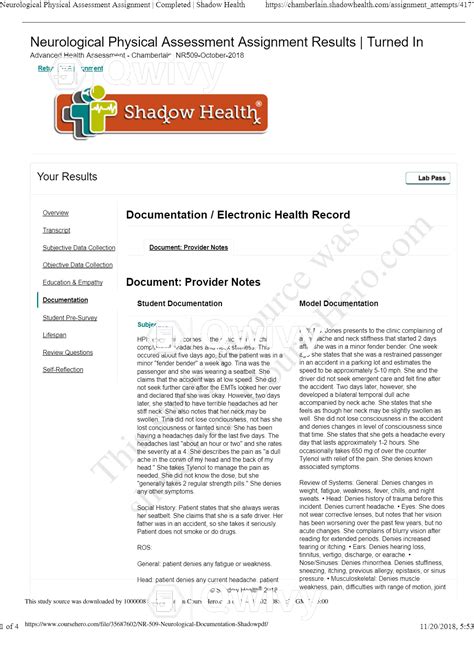
Table of Contents
Tina Jones Neurological Shadow Health Documentation: A Comprehensive Guide
Shadow Health Tina Jones Neurological assessment presents a valuable opportunity for nursing students to practice their neurological examination skills in a risk-free environment. This detailed guide will walk you through a comprehensive documentation approach, focusing on key findings, relevant nursing diagnoses, and appropriate interventions. We’ll explore how to document your findings effectively to meet the high standards of professional nursing practice. Mastering this crucial skill will enhance your confidence and prepare you for real-world clinical encounters.
Understanding the Neurological Assessment in Shadow Health
The Tina Jones neurological assessment in Shadow Health simulates a patient encounter, allowing you to practice various aspects of neurological assessment, including:
- Mental Status: Assessing level of consciousness, orientation, cognitive function, and mood. Look for signs of confusion, disorientation, or altered mental status.
- Cranial Nerves: Evaluating the function of the twelve cranial nerves, noting any deficits or abnormalities.
- Motor Function: Assessing muscle strength, tone, coordination, and involuntary movements. Observe for any tremors, weakness, or paralysis.
- Sensory Function: Testing various sensory modalities like touch, pain, temperature, vibration, and proprioception. Document any areas of sensory loss or impairment.
- Reflexes: Evaluating deep tendon reflexes (DTRs) and superficial reflexes. Note the presence or absence of reflexes, and their grading.
- Cerebellar Function: Assessing balance, coordination, and gait. Observe for any ataxia or incoordination.
Detailed Documentation of Key Findings: A Step-by-Step Approach
Effective documentation is crucial for clear communication and appropriate patient care. Here’s a structured approach to documenting your Tina Jones Neurological Shadow Health findings:
1. Subjective Data:
This section focuses on information gathered directly from the patient or from their chart, including:
- Chief Complaint: Clearly state the reason for the neurological assessment (e.g., headache, weakness, dizziness). Use direct quotes whenever possible. *Example: "Patient states, 'I've had a severe headache for the past three days.'" *
- History of Present Illness (HPI): Provide a detailed account of the onset, location, character, duration, severity, and associated symptoms of the patient's neurological concerns. This should follow the mnemonic OLD CART (Onset, Location, Duration, Character, Aggravating factors, Relieving factors, Timing). Example: "Patient reports a throbbing headache in the frontal region, lasting for 3 days, worsening with physical activity and relieved by rest. The patient denies any fever, nausea, or vomiting."
- Past Medical History (PMH): Note any relevant past medical conditions, such as stroke, head trauma, seizures, or neurological disorders. Include dates and treatment details.
- Medications: List all current medications, including over-the-counter drugs and herbal supplements. Note dosage and frequency.
- Allergies: Document any known allergies, including reactions.
- Family History: Note any family history of neurological disorders.
- Social History: Relevant social history might include alcohol and tobacco use, recreational drug use, and occupation.
2. Objective Data:
This section documents your findings from the physical examination. Use precise and factual language, avoiding subjective interpretations. Organize your findings systematically, following a standard neurological examination format:
- Mental Status:
- Level of Consciousness: Document the patient's level of alertness and responsiveness (e.g., alert and oriented x3 to person, place, and time; lethargic; stuporous; comatose).
- Cognitive Function: Assess attention span, memory (short-term and long-term), and cognitive abilities. Document any deficits.
- Cranial Nerves (CN): Document your assessment of each cranial nerve individually, noting any abnormalities. Example: "CN II-XII grossly intact." Be specific if any deficits are found.
- Motor Function:
- Muscle Strength: Grade muscle strength in each extremity using a standardized scale (e.g., 0-5 scale). Example: "Muscle strength 5/5 bilaterally in upper and lower extremities."
- Tone: Describe muscle tone (e.g., normal, hypotonic, hypertonic, spastic).
- Coordination: Assess coordination using finger-to-nose, heel-to-shin tests. Note any ataxia or dysmetria.
- Involuntary Movements: Document any tremors, fasciculations, or other involuntary movements.
- Sensory Function:
- Light Touch, Pain, Temperature: Assess sensation in all four extremities. Note any areas of hypoesthesia, hyperesthesia, or anesthesia.
- Vibration and Proprioception: Test vibration sense using a tuning fork. Assess proprioception by moving the patient's toes or fingers and asking them to identify the position.
- Reflexes:
- Deep Tendon Reflexes (DTRs): Grade DTRs using a standardized scale (e.g., 0-4+ scale). Document the response in each extremity (biceps, triceps, brachioradialis, patellar, Achilles). Example: "DTRs 2+ bilaterally."
- Superficial Reflexes: Assess superficial reflexes such as the plantar reflex (Babinski sign). Document the response.
- Cerebellar Function:
- Balance: Assess balance using Romberg test.
- Gait: Observe the patient's gait. Note any abnormalities (e.g., ataxia, spasticity, hemiparesis).
- Coordination: Assess rapid alternating movements (RAMs) and finger-to-nose testing.
3. Assessment:
This section involves formulating nursing diagnoses based on your findings. Use the NANDA-I nursing diagnoses taxonomy. Examples might include:
- Risk for falls: Due to impaired balance and coordination.
- Impaired physical mobility: Related to muscle weakness and ataxia.
- Acute pain: Related to headache.
- Impaired neurologic function: Related to [Specific neurological deficit].
- Deficient knowledge: Regarding neurological condition and management.
4. Plan:
This section outlines your planned interventions based on the nursing diagnoses. Include specific, measurable, achievable, relevant, and time-bound (SMART) goals. Examples might include:
- Pain Management: Administer analgesics as ordered, provide comfort measures, teach relaxation techniques.
- Fall Prevention: Implement fall risk precautions (bedside rails, call bell within reach), assist with ambulation, provide mobility aids as needed.
- Improve Mobility: Encourage regular range of motion exercises, assist with ambulation, provide physical therapy referral.
- Patient Education: Educate the patient and family about the neurological condition, medication regimen, and potential complications. Provide written materials as needed.
5. Evaluation:
This section describes the effectiveness of your interventions. Did the planned interventions achieve the stated goals? Document any changes in the patient’s condition and adjust the plan as needed. *Example: "Patient reports decreased headache pain after receiving analgesics. Patient ambulated with assistance and demonstrated improved balance." *
Addressing Common Neurological Findings in Tina Jones
Here's a brief overview of how to document some common neurological findings encountered in the Tina Jones simulation:
- Positive Babinski Sign: Document as "Upgoing plantar reflex (Babinski sign) present on the [right/left] side," indicating possible upper motor neuron lesion.
- Decreased Muscle Strength: Document the specific muscle group affected and the grade of muscle strength using the 0-5 scale.
- Abnormal Gait: Describe the specific abnormality (e.g., ataxic gait, spastic gait, antalgic gait).
- Sensory Loss: Specify the type of sensory loss (light touch, pain, temperature, vibration, proprioception) and the affected area(s).
- Abnormal Reflexes: Document the specific reflex and the grade of the response (e.g., hyperreflexia, hyporeflexia, absent reflexes).
Tips for Success in Shadow Health Tina Jones Neurological Assessment
- Thorough Preparation: Review relevant anatomy, physiology, and neurological examination techniques before starting the simulation.
- Systematic Approach: Follow a systematic approach to the neurological examination, ensuring you assess all key areas.
- Accurate Documentation: Use precise and concise language in your documentation. Pay attention to detail.
- Critical Thinking: Analyze your findings and formulate appropriate nursing diagnoses and interventions.
- Practice Makes Perfect: Practice the simulation multiple times to build your confidence and refine your skills.
By following this comprehensive guide, you can effectively document your findings in the Tina Jones Neurological Shadow Health simulation, fostering a deeper understanding of neurological assessment and preparing you for success in your nursing career. Remember, accurate and thorough documentation is paramount in providing safe and effective patient care.
Latest Posts
Latest Posts
-
Interactive Tutorial Forming Questions In Spanish
Mar 25, 2025
-
Correctly Match The Term And Description Bone Stem Cell
Mar 25, 2025
-
Although Some State Osha Programs Have Specified
Mar 25, 2025
-
Which Of The Following Is True Of A Research Proposal
Mar 25, 2025
-
The Characters In The Cask Of Amontillado
Mar 25, 2025
Related Post
Thank you for visiting our website which covers about Tina Jones Neurological Shadow Health Documentation . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
