Tina Jones Shadow Health Comprehensive Assessment
Onlines
Mar 15, 2025 · 7 min read
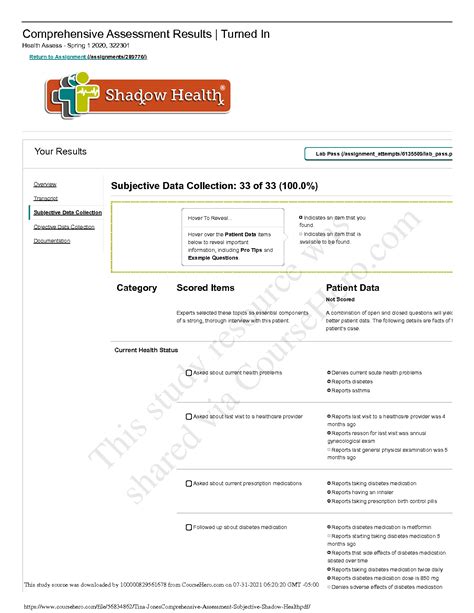
Table of Contents
Tina Jones Shadow Health Comprehensive Assessment: A Deep Dive
Shadow Health's Tina Jones case study provides nursing students with an invaluable opportunity to practice comprehensive assessment skills in a risk-free virtual environment. This detailed guide will walk you through a thorough assessment of Tina Jones, covering subjective and objective data, key findings, potential diagnoses, and the crucial nursing process involved. Mastering this virtual patient will significantly enhance your preparedness for real-world clinical encounters.
Subjective Data Collection: Listening to Tina Jones
The subjective data gathering phase is paramount. It involves actively listening to Tina Jones, asking pertinent questions, and meticulously documenting her responses. Remember, effective communication is key to building rapport and eliciting accurate information. Here are some key areas to focus on:
1. Identifying Data:
- Name: Tina Jones (This seems obvious, but accurate documentation starts here!)
- Age: (Check the provided patient data within the Shadow Health platform)
- Date of Birth: (Check the provided patient data)
- Occupation: (Check the provided patient data)
- Reason for Seeking Care: This is crucial. Pay close attention to Tina's chief complaint and the context surrounding it. This will guide your entire assessment.
2. History of Present Illness (HPI):
Thoroughly explore the details of Tina's current health concern. Use the mnemonic SAMPLE to structure your questioning:
- Symptoms: What are her specific symptoms? Describe their character, location, onset, duration, severity, and associated factors (e.g., pain, shortness of breath).
- Allergies: Document any known allergies, including the reaction experienced.
- Medications: List all current medications (prescription, over-the-counter, herbal supplements) including dosage, frequency, and duration of use.
- Past Medical History (PMH): Inquire about any previous illnesses, surgeries, or hospitalizations. This information is crucial in understanding Tina's overall health status and potential risk factors.
- Last Oral Intake (LOI): Note the time and type of food or fluids consumed. This is particularly relevant in certain clinical scenarios.
- Events: What events preceded the onset of her symptoms? This helps establish causality.
3. Past Medical, Surgical, and Family History:
- Past Medical History (PMH): Explore her history of illnesses, including childhood illnesses and any chronic conditions (e.g., hypertension, diabetes, asthma).
- Surgical History: Inquire about any previous surgeries and their outcomes.
- Family History: Document any significant illnesses in her immediate family members (parents, siblings, children). This can reveal potential genetic predispositions or familial risk factors.
4. Social History:
This aspect of the assessment is often overlooked, but it’s vital. Consider:
- Lifestyle: Does she smoke? Drink alcohol? Exercise regularly? What is her diet like? These factors significantly impact her overall health.
- Occupation: Does her work expose her to any hazards or stressors?
- Living Situation: Who does she live with? Does she have a supportive social network?
- Stress Levels: How is she coping with stress? Is she experiencing significant life changes or challenges?
5. Review of Systems (ROS):
Systematically review each body system. Even if Tina doesn't report symptoms in a particular system, you still need to document a negative finding. This is a comprehensive approach ensuring nothing is overlooked. Example areas include:
- General: Fever, chills, fatigue, weight changes.
- Skin: Rashes, lesions, itching.
- HEENT: Headache, eye pain, earache, nosebleeds, sore throat.
- Respiratory: Cough, shortness of breath, chest pain.
- Cardiovascular: Chest pain, palpitations, edema.
- Gastrointestinal: Nausea, vomiting, diarrhea, constipation, abdominal pain.
- Neurological: Headache, dizziness, weakness, numbness.
- Musculoskeletal: Joint pain, muscle aches, stiffness.
- Genitourinary: Urinary frequency, urgency, pain, vaginal discharge.
- Endocrine: Changes in weight, thirst, excessive urination.
- Psychosocial: Mental health status; mood, anxiety, depression.
Objective Data Collection: Performing the Physical Examination
After gathering subjective data, meticulously perform a physical examination. This involves utilizing your senses – sight, smell, hearing, and touch – to gather objective data. Remember to follow a systematic approach.
1. General Appearance:
- Level of consciousness: Alert, drowsy, lethargic, comatose?
- Appearance: Well-groomed, disheveled, anxious, distressed?
- Posture: Upright, slumped, guarded?
- Vital Signs: Temperature, pulse, respirations, blood pressure, oxygen saturation (SpO2). Note any abnormalities and their clinical significance.
2. HEENT Examination:
- Head: Inspect for symmetry, masses, tenderness. Palpate the scalp for lesions or tenderness.
- Eyes: Assess visual acuity, pupillary response, conjunctiva, sclera.
- Ears: Assess hearing acuity, inspect the external ear canal for cerumen or lesions.
- Nose: Assess patency of the nasal passages, inspect the nasal mucosa.
- Throat: Inspect the oral mucosa, tonsils, pharynx for redness, inflammation, or exudates.
3. Neck Examination:
- Lymph Nodes: Palpate for enlarged or tender lymph nodes.
- Thyroid: Assess for enlargement or nodules.
- Trachea: Assess for midline position.
- Jugular Venous Pressure (JVP): Assess for distention.
4. Respiratory Examination:
- Inspection: Observe respiratory rate, rhythm, depth, and use of accessory muscles.
- Palpation: Palpate the chest wall for tenderness, masses, or crepitus.
- Percussion: Percuss the lung fields for resonance or dullness.
- Auscultation: Auscultate the lung fields for breath sounds (normal, adventitious), and note any abnormalities.
5. Cardiovascular Examination:
- Inspection: Observe for jugular venous distention, pulsations, edema.
- Palpation: Palpate the apical impulse, assess for thrills or heaves.
- Auscultation: Auscultate the heart sounds (S1, S2, S3, S4, murmurs) at all auscultatory areas.
6. Abdominal Examination:
- Inspection: Observe the abdomen for distention, scars, masses, or pulsations.
- Auscultation: Auscultate bowel sounds in all four quadrants.
- Percussion: Percuss the abdomen for tympany or dullness.
- Palpation: Palpate the abdomen for tenderness, masses, or organomegaly. Start with light palpation and progress to deep palpation if indicated.
7. Neurological Examination:
- Mental Status: Assess level of consciousness, orientation, memory, cognitive function.
- Cranial Nerves: Assess the function of cranial nerves II-XII.
- Motor System: Assess muscle strength, tone, coordination.
- Sensory System: Assess light touch, pain, temperature, vibration, proprioception.
- Reflexes: Assess deep tendon reflexes.
8. Skin Examination:
Inspect the skin for color, temperature, moisture, turgor, lesions, and any other abnormalities.
9. Musculoskeletal Examination:
Assess the range of motion, strength, and any pain or limitations in the joints and muscles.
Remember to document all your findings meticulously, including normal and abnormal observations. Use precise and accurate terminology.
Key Findings and Potential Diagnoses in Tina Jones' Case
The specific findings in Tina Jones' case will vary depending on the scenario presented by the Shadow Health platform. However, some common areas of focus might include:
- Respiratory System: Assess for signs of infection (e.g., increased respiratory rate, diminished breath sounds, crackles or wheezes).
- Cardiovascular System: Evaluate for signs of hypertension, tachycardia, or murmurs.
- Gastrointestinal System: Check for abdominal pain, tenderness, or altered bowel sounds.
- Neurological System: Evaluate mental status, level of consciousness, and motor function.
- Musculoskeletal System: Assess joint pain, swelling, or limited range of motion.
Based on your findings, you should be able to formulate potential diagnoses. Remember to consider the patient's history, risk factors, and the clinical presentation. This requires a critical thinking approach. The goal is not to definitively diagnose but to identify potential problems requiring further investigation and management.
The Nursing Process: Planning, Implementing, and Evaluating
Once you've gathered subjective and objective data and formulated potential diagnoses, the nursing process guides your actions:
1. Planning:
Based on your assessment findings, develop a plan of care that addresses Tina's immediate needs and promotes her overall well-being. This plan should include specific, measurable, achievable, relevant, and time-bound (SMART) goals. Prioritize actions based on urgency and clinical significance.
2. Implementing:
This involves carrying out the planned interventions. In the Shadow Health simulation, this might include:
- Administering medications: Select the appropriate medications and dosages based on the simulation's guidelines.
- Educating the patient: Provide Tina with information about her condition, treatment plan, and self-care strategies.
- Monitoring vital signs: Closely monitor Tina's vital signs to detect changes and intervene accordingly.
- Performing assessments: Repeat assessments to track progress and detect any changes in her condition.
3. Evaluating:
Continuously evaluate the effectiveness of your interventions. Did your actions achieve the desired outcomes? If not, you need to adjust your plan of care accordingly. This cyclical nature of the nursing process is crucial.
Utilizing Shadow Health for Optimal Learning
Shadow Health’s Tina Jones case study offers a unique opportunity to refine your clinical skills. To maximize your learning:
- Practice Active Listening: Pay close attention to what Tina says, both verbally and nonverbally.
- Ask Clarifying Questions: Don't hesitate to ask clarifying questions to ensure you understand Tina’s concerns and symptoms.
- Document Thoroughly: Meticulous documentation is vital for effective communication and continuity of care.
- Reflect on Your Actions: After completing the assessment, take time to reflect on your performance. What did you do well? Where could you improve?
- Repeat the Scenario: Don't be afraid to repeat the scenario multiple times. Each repetition provides a valuable opportunity to refine your skills and confidence.
By mastering the Tina Jones case study, you’ll significantly enhance your clinical judgment, communication skills, and overall preparedness for real-world patient care. Remember, practice makes perfect, and Shadow Health provides an invaluable platform for honing your nursing skills. Utilize every opportunity to learn, grow, and refine your approach to patient assessment and care.
Latest Posts
Latest Posts
-
Meet The Muscles Muscle Anatomy Workbook
Mar 15, 2025
-
Lesson 13 2 Learning The Key Terms
Mar 15, 2025
-
House On Mango Street Summary Of Each Chapter
Mar 15, 2025
-
Mi Madre 1 Of 1 Compra Ropa Fea A Mi
Mar 15, 2025
-
Being Willing To Adapt To And Learn New Technology Will
Mar 15, 2025
Related Post
Thank you for visiting our website which covers about Tina Jones Shadow Health Comprehensive Assessment . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
