Translate The Medical Term Cochleitis As Literally As Possible.
Onlines
Mar 06, 2025 · 8 min read
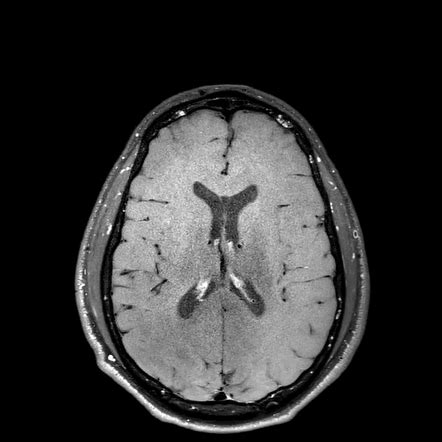
Table of Contents
A Deep Dive into Cochleitis: A Literal Translation and Exploration
The term "cochleitis" might seem daunting to the uninitiated, conjuring images of complex medical procedures and intricate anatomy. Let's unravel its meaning, explore its literal translation, and delve into the condition itself to provide a comprehensive understanding accessible to both medical professionals and the general public.
Understanding the Components: Cochlea and -itis
Before tackling the literal translation, let's dissect the word "cochleitis" into its core components. This approach allows for a more nuanced grasp of its meaning and clinical implications.
The Cochlea: The Snail-Shaped Wonder
The word "cochlea" originates from the Greek word "κοχλίας" (kochlias), meaning "snail." This is a highly apt descriptor, as the cochlea is a spiral-shaped, fluid-filled structure residing within the inner ear. Its snail-like form is crucial to its function. Think of it as a highly specialized organ responsible for transforming sound vibrations into neural signals that the brain can interpret as sound. Within the cochlea, we find the Organ of Corti, a remarkable structure containing hair cells—the sensory receptors that are essential for hearing. Damage to these hair cells, often from excessive noise exposure, aging, or certain medical conditions, leads to hearing loss.
The Suffix "-itis": Inflammation Takes Center Stage
The suffix "-itis" is a common medical term indicating inflammation. In various contexts, "-itis" denotes the presence of inflammation in a specific body part or organ. For instance, appendicitis refers to inflammation of the appendix, tonsillitis refers to inflammation of the tonsils, and so on. In "cochleitis," the suffix "-itis" clearly indicates that the inflammation is localized within the cochlea itself.
Literal Translation of Cochleitis: Inflammation of the Cochlea
Therefore, a literal translation of "cochleitis" would be inflammation of the cochlea. It's a straightforward and accurate depiction of the condition. The term precisely points to the location (cochlea) and the underlying pathological process (inflammation). This clarity is critical for both accurate medical communication and patient understanding.
The Clinical Picture of Cochleitis: Symptoms and Diagnosis
While the literal translation provides a foundational understanding, a deeper exploration into the clinical manifestation of cochleitis is crucial. The symptoms, diagnostic methods, and potential treatments paint a more complete picture of this intricate condition.
Recognizing the Warning Signs: Symptoms of Cochleitis
The symptoms of cochleitis can vary depending on the severity and underlying cause of the inflammation. However, some common signs include:
-
Sensorineural Hearing Loss: This is often the most prominent symptom, characterized by a reduction in the ability to hear sounds, particularly at certain frequencies. It differs from conductive hearing loss, which is caused by problems with the outer or middle ear. Sensorineural hearing loss results from damage to the inner ear structures, specifically the hair cells within the cochlea.
-
Tinnitus: This manifests as a persistent ringing, buzzing, hissing, or clicking sound in one or both ears. The perceived sound can vary in intensity and pitch, and it can be extremely disruptive to daily life. Tinnitus is often a hallmark of inner ear disorders, including cochleitis.
-
Dizziness and Vertigo: While not always present, dizziness or vertigo (a sensation of spinning or movement) can accompany cochleitis, suggesting involvement of the vestibular system, which is closely associated with the cochlea within the inner ear. This symptom underscores the interconnectedness of the structures within the inner ear.
-
Aural Fullness: This refers to a feeling of pressure or fullness in the ear, as if the ear is blocked or plugged.
Unveiling the Diagnosis: Investigative Techniques
Diagnosing cochleitis requires a careful and systematic approach, utilizing various diagnostic techniques to pinpoint the underlying cause and extent of the inflammation. Some common methods include:
-
Audiometry: This is a crucial test that measures hearing sensitivity at different frequencies. Audiometric results can help differentiate between conductive and sensorineural hearing loss, providing critical information about the location and nature of the hearing impairment.
-
Tympanometry: This test assesses the function of the middle ear. While not directly assessing the cochlea, tympanometry helps rule out middle ear problems that could mimic the symptoms of cochleitis.
-
Acoustic Reflex Testing: This test examines the reflex contraction of the middle ear muscles in response to loud sounds. Abnormal acoustic reflexes can indicate problems within the auditory pathway, including the cochlea.
-
Otoacoustic Emissions (OAEs): This non-invasive test measures sounds produced by the inner ear. Absent or abnormal OAEs can suggest damage to the hair cells within the cochlea.
-
Auditory Brainstem Response (ABR): ABR is an electrophysiological test that measures the electrical activity of the auditory nerve and brainstem in response to sounds. This test helps assess the integrity of the auditory pathway from the cochlea to the brainstem.
-
Magnetic Resonance Imaging (MRI): While not routinely used for cochlear inflammation, MRI can be helpful in ruling out other conditions that may mimic the symptoms of cochleitis, such as tumors or other structural abnormalities in the inner ear.
Treatment Strategies: Managing and Mitigating Cochleitis
The treatment of cochleitis depends on the underlying cause and the severity of the symptoms. Unfortunately, there's no universally effective cure for all types of cochlear inflammation. However, treatments aim to manage symptoms, prevent further damage, and improve the patient's quality of life.
-
Medications: Depending on the suspected cause, medications like corticosteroids (anti-inflammatory drugs) may be prescribed to reduce inflammation. Antiviral medications might be used if a viral infection is implicated. Pain relievers can alleviate discomfort associated with inflammation.
-
Hearing Aids: For patients experiencing significant hearing loss, hearing aids can help amplify sounds and improve communication. Hearing aids are often a crucial component of managing the functional consequences of cochleitis.
-
Cochlear Implants: In severe cases of sensorineural hearing loss where hearing aids provide insufficient benefit, a cochlear implant may be considered. This surgically implanted device bypasses the damaged hair cells and directly stimulates the auditory nerve.
-
Tinnitus Management: Strategies for managing tinnitus include sound therapy, counseling, and cognitive behavioral therapy. These methods aim to reduce the distress associated with tinnitus and improve the patient's ability to cope with this persistent sound.
-
Lifestyle Modifications: In some cases, lifestyle changes may be recommended to reduce the risk of further damage. This may include limiting exposure to loud noises, avoiding certain medications known to affect hearing, and managing underlying medical conditions.
Causes and Risk Factors: Understanding the Etiology
The causes of cochleitis are diverse and not always clearly understood. However, several factors have been associated with an increased risk of developing this condition.
-
Viral Infections: Viral infections, such as the influenza virus or mumps virus, can sometimes cause inflammation in the inner ear, leading to cochleitis.
-
Bacterial Infections: Bacterial infections can also contribute to inner ear inflammation. This often occurs as a complication of middle ear infections (otitis media) that spread to the inner ear.
-
Autoimmune Diseases: In some cases, cochleitis may be related to autoimmune diseases, where the body's immune system mistakenly attacks its own tissues, including the cochlea.
-
Traumatic Injury: Head injuries or other forms of trauma can damage the delicate structures of the inner ear, leading to inflammation and hearing loss.
-
Exposure to Ototoxic Drugs: Certain medications, such as some antibiotics and chemotherapy drugs, are known to be ototoxic, meaning they can damage the inner ear and contribute to cochleitis.
-
Genetic Factors: Genetic predisposition may play a role in the susceptibility to certain types of cochleitis.
-
Noise-Induced Hearing Loss: Prolonged exposure to loud noise can damage hair cells in the cochlea, leading to hearing loss and potentially inflammation.
Differentiating Cochleitis from Other Inner Ear Conditions
It's crucial to differentiate cochleitis from other inner ear conditions that share similar symptoms. Accurate diagnosis is vital for appropriate treatment. Conditions that can sometimes mimic cochleitis include:
-
Ménière's Disease: This inner ear disorder is characterized by episodes of vertigo, tinnitus, hearing loss, and a sensation of fullness in the ear. While there might be overlap in symptoms, Ménière's Disease involves the entire inner ear, while cochleitis primarily affects the cochlea.
-
Labyrinthitis: This condition involves inflammation of the labyrinth, the inner ear structure responsible for both hearing and balance. Labyrinthitis typically presents with more pronounced vertigo than cochleitis.
-
Acoustic Neuroma: This is a benign tumor that grows on the vestibulocochlear nerve, which carries auditory and balance information from the inner ear to the brain. An acoustic neuroma can cause hearing loss, tinnitus, and dizziness, but it is a distinct entity from cochleitis.
Conclusion: A Holistic View of Cochleitis
In conclusion, "cochleitis" literally translates to inflammation of the cochlea. This seemingly simple phrase encapsulates a complex medical condition involving inflammation of the intricate, snail-shaped structure responsible for hearing. The symptoms, diagnostic approaches, treatment strategies, and underlying causes discussed in this article provide a comprehensive understanding of this condition. Early diagnosis and appropriate management are crucial for mitigating the impact of cochleitis on hearing and overall quality of life. While a complete cure may not always be possible, effective management strategies exist to minimize the effects of this inner ear disorder. Further research continues to improve our understanding and treatment options for this often debilitating condition.
Latest Posts
Latest Posts
-
Energy Pyramids Tying It All Together
Mar 06, 2025
-
Compared To The Netherlands Egypt Has
Mar 06, 2025
-
While Reviewing Clinical Notes With Replacement Nurses
Mar 06, 2025
-
Advance Study Assignment Densities Of Solids And Liquids
Mar 06, 2025
-
Your New Material May Aggregate Or Bring Together
Mar 06, 2025
Related Post
Thank you for visiting our website which covers about Translate The Medical Term Cochleitis As Literally As Possible. . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
