Vulvar Cancer In Situ Can Also Be Documented As
Onlines
Mar 17, 2025 · 7 min read
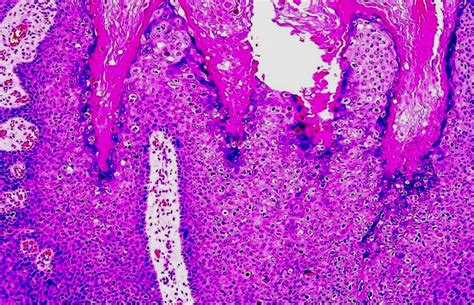
Table of Contents
Vulvar Cancer In Situ: Understanding the Terminology and Implications
Vulvar cancer in situ, also known by several other terms, represents a critical area of understanding in gynecological oncology. This condition, characterized by abnormal cell growth confined to the vulvar surface, is crucial to diagnose early for successful treatment and improved patient outcomes. This article delves deep into the various ways vulvar cancer in situ can be documented, clarifying the terminology and its implications for diagnosis, treatment, and prognosis.
Synonyms and Alternative Terminology for Vulvar Cancer In Situ
The medical documentation of vulvar cancer in situ employs a variety of terms, often reflecting the specific histological findings or the stage of the disease. Understanding these synonyms is crucial for healthcare professionals and patients alike. These terms are frequently used interchangeably, but subtle differences can exist depending on the context.
1. Intraepithelial Neoplasia (VIN):
This is perhaps the most common alternative term. VIN encompasses various degrees of cellular abnormality within the vulvar epithelium. It's further categorized into:
- VIN 1 (Mild dysplasia): Characterized by minimal cellular changes and a low risk of progression to invasive cancer.
- VIN 2 (Moderate dysplasia): Shows more significant cellular abnormalities with an increased risk of progression.
- VIN 3 (Severe dysplasia/Carcinoma in situ): Exhibits the most pronounced cellular changes and is considered the most likely to progress to invasive cancer if left untreated. This is often the stage where the term "carcinoma in situ" is used more explicitly.
2. Carcinoma in Situ (CIS):
This term specifically implies that abnormal cells are confined to the surface layers of the vulva, without invasion into deeper tissues. It represents a pre-invasive stage, emphasizing the potential for progression to invasive cancer. However, it's crucial to remember that even though it's "in situ," it requires careful monitoring and often treatment.
3. Bowen's Disease:
This refers to a specific type of vulvar intraepithelial neoplasia (VIN) with a characteristic histological appearance. It's often characterized by a well-defined, reddish-brown plaque or lesion on the vulva. It's considered a form of VIN 3 or carcinoma in situ.
4. Paget's Disease of the Vulva:
While sharing the name, this is distinctly different from Bowen's disease and other VIN subtypes. Paget's disease of the vulva involves abnormal cells that resemble Paget cells, typically associated with adenocarcinoma. It can be associated with underlying invasive or in situ adenocarcinoma of the vulva or other related structures. This requires a different diagnostic approach and treatment strategy.
Understanding the Implications of Each Term
While these terms are often used interchangeably, understanding the nuances is critical for patient care. For example, a diagnosis of VIN 1 carries a lower risk of progression than VIN 3. The term "carcinoma in situ," while implying a pre-invasive state, highlights the potential for malignant transformation and the need for prompt intervention.
The significance of precise terminology lies in:
- Risk stratification: Accurate classification helps clinicians assess the risk of progression to invasive cancer and tailor treatment accordingly.
- Treatment planning: The choice of treatment (e.g., observation, local excision, or more extensive surgery) is directly influenced by the specific diagnosis and grade of VIN.
- Prognostication: Knowing the subtype of VIN allows for a more accurate prediction of long-term outcomes and the need for surveillance.
- Communication: Clear and consistent use of terminology ensures effective communication between healthcare providers, researchers, and patients.
Diagnostic Procedures for Vulvar Cancer In Situ
Accurate diagnosis of vulvar cancer in situ is crucial. This involves a combination of techniques:
- Physical examination: A thorough examination of the vulva by a gynecologist is the first step. This may reveal suspicious lesions.
- Biopsy: This is the gold standard for diagnosis. A small tissue sample is taken from the suspicious area and examined under a microscope to confirm the presence of abnormal cells and determine the grade of VIN.
- Colposcopy: This procedure uses a magnifying instrument to visualize the vulvar surface, allowing for precise biopsy targeting.
- Imaging: While typically not needed for in situ cancers, imaging techniques such as MRI or CT scans might be used if there's a suspicion of deeper invasion.
Treatment Options for Vulvar Cancer In Situ
Treatment options for vulvar cancer in situ vary depending on factors such as the extent of the disease, the patient's age and overall health, and personal preferences.
- Observation: For some low-grade VIN (VIN 1) lesions, close observation and regular follow-up may be an option. However, this requires careful monitoring for any changes.
- Local excision: This surgical procedure removes the abnormal tissue. The extent of surgery depends on the size and location of the lesion.
- Wide local excision: This involves removing a larger area of tissue surrounding the lesion, often used for larger or more concerning lesions.
- Laser ablation: This technique uses a laser to destroy abnormal cells.
- Cryotherapy: This method uses freezing to destroy abnormal cells.
- Topical treatments: In certain cases, topical medications such as imiquimod might be used.
Long-Term Follow-up and Surveillance
After treatment, regular follow-up appointments are crucial. This includes:
- Physical examinations: To monitor for recurrence or new lesions.
- Colposcopy: Periodic colposcopic examinations to assess for any signs of disease.
- Biopsies: If any suspicious lesions are found, biopsies are performed to confirm their nature.
The frequency of follow-up depends on the type and extent of treatment, as well as the individual patient's risk factors.
The Importance of Early Detection and Prevention
Early detection is paramount in improving outcomes for vulvar cancer in situ. Regular gynecological examinations, including pelvic exams and visual inspection of the vulva, are essential. Women who notice any changes in the appearance of their vulva, such as unusual growths, sores, or discoloration, should consult their doctor immediately.
While there are no definitive preventative measures, minimizing risk factors such as smoking, human papillomavirus (HPV) infection, and certain chronic skin conditions can contribute to a reduced risk. HPV vaccination is recommended for young girls and women to prevent HPV-related cancers, including vulvar cancer.
Living with Vulvar Cancer In Situ: Emotional and Psychological Well-being
A diagnosis of vulvar cancer in situ can be emotionally challenging. Fear, anxiety, and uncertainty are common reactions. It's crucial for patients to have access to support systems, including:
- Medical professionals: Open communication with oncologists, gynecologists, and other healthcare providers is vital.
- Support groups: Connecting with other women who have experienced similar diagnoses can provide invaluable emotional support and practical advice.
- Mental health professionals: Counseling or therapy can assist in coping with emotional distress and improving overall well-being.
Open and honest communication with healthcare providers and loved ones is crucial for navigating the emotional and practical challenges associated with a diagnosis of vulvar cancer in situ.
Research and Future Directions
Ongoing research continues to refine our understanding of vulvar cancer in situ, including:
- Improved diagnostic techniques: Researchers are exploring new methods to enhance the accuracy and efficiency of diagnosing VIN.
- Targeted therapies: Efforts are focused on developing targeted therapies that specifically attack abnormal cells while minimizing damage to healthy tissue.
- Risk prediction models: Researchers are working on developing more accurate models to predict the risk of progression to invasive cancer.
- Prevention strategies: Ongoing research explores ways to prevent HPV infection and other risk factors associated with vulvar cancer.
Conclusion: Navigating the Terminology and Ensuring Optimal Outcomes
Vulvar cancer in situ, whether documented as VIN, CIS, Bowen's disease, or other related terms, demands careful attention and timely intervention. Understanding the nuances of the terminology, the diagnostic procedures, treatment options, and the importance of long-term follow-up is critical for ensuring the best possible patient outcomes. Early detection, effective treatment, and strong emotional support are key elements in successfully managing this condition and maintaining a high quality of life. The ongoing research promises even better diagnostic and therapeutic approaches in the future. Remember, open communication with your healthcare team and access to supportive resources are essential throughout your journey.
Latest Posts
Latest Posts
-
Unit 3 Progress Check Frq Part A Ap Calculus
Mar 18, 2025
-
A Long Way Gone Chapter Notes
Mar 18, 2025
-
Lt F12 Giant Eye With Eyelid And Lacrimal System
Mar 18, 2025
-
Resources And Tools For Innovative Practices In An Easily Digestible
Mar 18, 2025
-
Kira A Project Manager Needs To Book
Mar 18, 2025
Related Post
Thank you for visiting our website which covers about Vulvar Cancer In Situ Can Also Be Documented As . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
