What Assessment Finding Is Consistent With Impending Herniation Syndrome
Onlines
Mar 10, 2025 · 7 min read
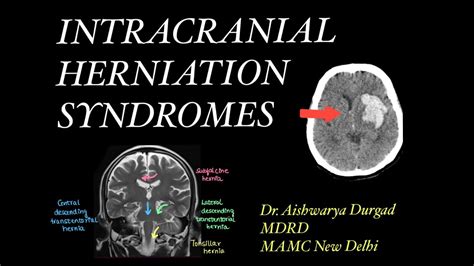
Table of Contents
What Assessment Findings Are Consistent with Impending Herniation Syndrome?
Impending herniation syndrome, a critical neurological emergency, signifies the brain's imminent shift due to increased intracranial pressure (ICP). Early and accurate recognition is paramount for prompt intervention, potentially preventing irreversible neurological damage or death. This article will delve into the crucial assessment findings consistent with this life-threatening condition, highlighting their significance in diagnosis and management.
Understanding Intracranial Pressure and Herniation
Before exploring the assessment findings, it's essential to grasp the underlying pathophysiology. The cranium, a rigid bony structure, houses the brain, cerebrospinal fluid (CSF), and blood. These components maintain a delicate equilibrium; any disruption can lead to increased ICP. When ICP surpasses the brain's capacity to compensate, herniation occurs—the displacement of brain tissue through the openings in the skull's base. This herniation compromises blood supply and function to various brain regions, resulting in severe neurological deficits.
Factors Contributing to Increased ICP and Herniation
Several factors can elevate ICP, paving the way for herniation. These include:
- Brain tumors: Expanding masses exert pressure on surrounding brain tissue.
- Cerebral hemorrhage: Bleeding within the brain significantly increases intracranial volume.
- Cerebral edema: Swelling of brain tissue, often due to trauma, infection, or ischemia.
- Head injuries: Traumatic brain injuries (TBIs) can cause bleeding, edema, and tissue damage.
- Meningitis and encephalitis: Infections of the brain and meninges lead to inflammation and swelling.
- Abscesses: Localized collections of pus within the brain.
- Hydrocephalus: Accumulation of CSF within the ventricles of the brain.
Clinical Manifestations of Impending Herniation: A Detailed Examination
Recognizing the signs and symptoms of impending herniation is critical. These often progress gradually, but can also appear suddenly and dramatically. A comprehensive neurological assessment is imperative.
1. Altered Level of Consciousness (LOC):
This is often the earliest and most significant indicator. Changes can range from subtle drowsiness and confusion to profound coma. Decreased responsiveness, delayed verbal responses, and difficulty maintaining arousal should raise immediate concern. Assess LOC using the Glasgow Coma Scale (GCS), a widely used tool for quantifying neurological impairment. A decreasing GCS score signifies neurological deterioration.
2. Pupillary Changes:
Pupillary responses are highly sensitive indicators of brainstem compression. Unilateral or bilateral pupillary dilation (mydriasis) suggests compression of the oculomotor nerve (CN III). Fixed and dilated pupils are a grave sign, indicating severe brainstem compression and impending respiratory arrest. Asymmetrical pupillary responses should also be considered a warning sign. Observe for sluggish or absent pupillary light reflexes.
3. Motor Dysfunction:
Assess motor strength and function in all four extremities. Weakness, hemiparesis (weakness on one side of the body), or hemiplegia (paralysis on one side of the body) suggest involvement of the motor cortex or corticospinal tracts. Decerebrate posturing (extension of the extremities) and decorticate posturing (flexion of the upper extremities and extension of the lower extremities) represent severe brainstem dysfunction. These abnormal postures are ominous signs indicating significant neurological compromise. Observe for any involuntary movements, such as clonus (rhythmic muscle contractions) or tremors.
4. Respiratory Pattern Changes:
Changes in breathing patterns reflect brainstem involvement. Irregular breathing patterns, such as Cheyne-Stokes respiration (alternating periods of apnea and hyperventilation) and apneustic breathing (prolonged inspiratory pauses), are indicative of severe brainstem compression. Ataxic breathing, characterized by completely irregular respiratory patterns, is an extremely grave finding. Monitor respiratory rate, rhythm, and depth closely. Respiratory arrest is a potentially fatal complication.
5. Vital Sign Alterations:
- Hypertension: Increased ICP often triggers a rise in blood pressure, a compensatory mechanism to maintain cerebral perfusion. Observe for widened pulse pressure (the difference between systolic and diastolic blood pressure).
- Bradycardia: As ICP rises, the vagal nerve may be stimulated, leading to a decrease in heart rate. This is part of the Cushing's triad.
- Bradypnea: Slowed respiratory rate may also be present, often as part of Cushing's triad.
- Cushing's Triad: The combination of hypertension, bradycardia, and bradypnea is a late and ominous sign indicating severe brainstem compression and impending herniation. This is a medical emergency requiring immediate intervention.
6. Vomiting:
Persistent and projectile vomiting, often unrelated to food intake, can be a manifestation of increased ICP. It's due to stimulation of the vomiting center in the brainstem.
7. Headache:
Severe, unrelenting headaches, particularly those accompanied by other neurological signs, should raise suspicion of increased ICP. The headache is often described as worsening and may be accompanied by nausea and vomiting.
8. Visual Disturbances:
Blurred vision, diplopia (double vision), or visual field deficits can indicate compression of the visual pathways or cranial nerves.
9. Seizures:
Seizures can occur as a result of the underlying cause of increased ICP or as a direct consequence of herniation.
Differentiating Impending Herniation from Other Conditions
It's crucial to distinguish impending herniation from other conditions with similar symptoms, such as:
- Stroke: Although stroke can cause neurological deficits, the pattern of impairment usually differs from that of impending herniation. Imaging studies are crucial for differentiation.
- Metabolic encephalopathy: Conditions like hypoglycemia, hepatic encephalopathy, and uremia can mimic some aspects of herniation, but their underlying causes are metabolic rather than structural.
- Drug overdose or intoxication: Substance abuse can affect neurological function, and careful assessment is needed to rule out intoxication.
Diagnostic Investigations: Confirming the Suspicion
Clinical assessment alone is insufficient to definitively diagnose impending herniation. Several diagnostic tools are essential:
- Computed Tomography (CT) scan: CT provides rapid visualization of brain structures and identifies the presence of bleeding, edema, tumors, or other space-occupying lesions. It's the initial imaging modality of choice.
- Magnetic Resonance Imaging (MRI): MRI offers superior visualization of brain tissue and can help identify subtle abnormalities not detectable on CT.
- Intracranial Pressure (ICP) monitoring: Direct measurement of ICP using an intracranial pressure monitor is crucial in managing patients at high risk of herniation. This provides continuous monitoring of ICP and facilitates early intervention.
Management of Impending Herniation: A Multifaceted Approach
Management of impending herniation is a time-critical, multifaceted endeavor requiring an interdisciplinary team approach. Treatment focuses on reducing ICP, addressing the underlying cause, and providing supportive care.
Key interventions:
- Hyperventilation: Controlled hyperventilation reduces PaCO2, causing cerebral vasoconstriction and decreased ICP. However, prolonged hyperventilation can be detrimental and should be carefully managed.
- Osmotherapy (Mannitol, Hypertonic Saline): These agents reduce cerebral edema by drawing fluid from the brain tissue into the vascular compartment.
- Steroids (Dexamethasone): In certain cases, corticosteroids are used to reduce cerebral edema, although their efficacy is controversial and they carry potential risks.
- Surgical intervention: Depending on the underlying cause, surgery may be necessary to remove a hematoma, tumor, or abscess. Placement of an external ventricular drain (EVD) may be required to lower ICP.
- Supportive care: Maintaining adequate airway, oxygenation, and hemodynamic stability is crucial. Careful monitoring of vital signs, neurological status, and ICP is essential.
Prognosis: A Dependent Factor
The prognosis for patients with impending herniation is highly variable and depends on various factors, including:
- The underlying cause: Some causes, such as a small ischemic stroke, might have better outcomes compared to a massive intracranial bleed.
- Severity of ICP elevation: The higher the ICP and the longer it persists, the worse the prognosis.
- Speed and effectiveness of treatment: Prompt diagnosis and appropriate management significantly improve the chance of survival and neurological recovery.
- Pre-existing medical conditions: Patients with pre-existing health problems may have a more difficult recovery.
Conclusion: A Call for Vigilance
Impending herniation syndrome is a critical neurological emergency demanding prompt recognition and intervention. Early identification of the characteristic assessment findings discussed above is crucial for timely management. A high index of suspicion is essential in patients presenting with altered LOC, pupillary changes, motor dysfunction, respiratory pattern abnormalities, and vital sign alterations. The collaborative efforts of neurologists, neurosurgeons, and other healthcare professionals are critical in minimizing morbidity and mortality associated with this potentially fatal condition. Continued research and advancements in diagnostic tools and treatment strategies hold promise for improving outcomes in this challenging clinical scenario. Further research is needed to improve our understanding of the subtle early markers and refine our treatment protocols. Ultimately, proactive monitoring, rapid diagnosis, and aggressive management are key determinants of survival and functional outcome in individuals facing the threat of impending herniation.
Latest Posts
Latest Posts
-
Basic Communication Crossword Notes Puzzle Answers
Mar 10, 2025
-
How Do You Individualize A Patients Care Plan In Epic
Mar 10, 2025
-
Rising Action Examples In Helen Keller
Mar 10, 2025
-
A Nurse Is Preparing To Administer Esomeprazole 40 Mg
Mar 10, 2025
-
Select All The Descriptions About Art And The Sacred Realm
Mar 10, 2025
Related Post
Thank you for visiting our website which covers about What Assessment Finding Is Consistent With Impending Herniation Syndrome . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
