Which Action Is Not Part Of The Acute Stroke Pathway
Onlines
Mar 06, 2025 · 5 min read
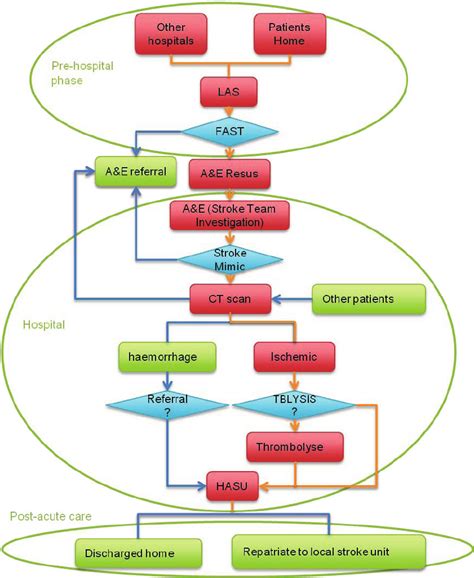
Table of Contents
Which Action is NOT Part of the Acute Stroke Pathway? A Comprehensive Guide
Stroke, a devastating neurological event caused by interrupted blood flow to the brain, demands immediate and precise action. The Acute Stroke Pathway (ASP) is a carefully designed, time-sensitive protocol aimed at minimizing long-term disability and improving patient outcomes. Understanding what constitutes the ASP, and equally importantly, what doesn't, is crucial for healthcare professionals and the public alike. This article will delve deep into the ASP, highlighting actions that are definitively not part of the established pathway.
The Core Principles of the Acute Stroke Pathway
Before examining actions excluded from the ASP, let's briefly review its core tenets. The ASP's success hinges on speed and efficiency:
- Rapid Recognition and Triage: Early identification of stroke symptoms is paramount. This involves swift assessment by emergency medical services (EMS), hospital staff, and even by individuals recognizing signs in others.
- Timely Imaging: Neuroimaging, typically CT or MRI scans, is crucial to differentiate between ischemic stroke (blocked artery) and hemorrhagic stroke (bleeding in the brain). This informs treatment choices.
- Prompt Treatment: For ischemic stroke, the most effective treatment is intravenous thrombolysis (IV tPA), a clot-busting drug. This must be administered within a specific timeframe (typically within 4.5 hours of symptom onset, though this can be extended in certain cases). For hemorrhagic stroke, management focuses on controlling bleeding and reducing pressure on the brain.
- Ongoing Neurological Monitoring: Continuous monitoring of the patient's neurological status is essential to track progress and detect any deterioration.
- Rehabilitation Planning: Early initiation of rehabilitation planning, even during the acute phase, helps optimize long-term recovery.
Actions NOT Included in the Acute Stroke Pathway
Several actions are explicitly excluded from, or directly contradict, the efficient and effective implementation of the ASP. These actions can significantly delay treatment, compromise patient safety, and worsen outcomes. Let's examine some key examples:
1. Unnecessary Delays in Transport and Assessment
Anything that delays getting the stroke patient to a stroke center capable of providing the full ASP is a critical error. This includes:
- Prolonged pre-hospital delays: Unnecessary stops, lengthy evaluations at non-stroke-capable facilities, or inefficient EMS response times all contribute to delays. Time is brain; every minute counts.
- Inefficient hospital triage: Failure to prioritize stroke patients within the emergency department (ED) can lead to substantial delays in imaging and treatment. The ASP requires a streamlined system for rapid assessment and prioritization.
- Unnecessary investigations: Performing non-essential tests before crucial imaging (CT scan) is a major impediment. The focus must remain on confirming the diagnosis of stroke and initiating appropriate treatment.
2. Inappropriate Treatment Decisions
Certain actions, even if well-intentioned, can be harmful and are outside the ASP:
- Delaying or foregoing CT scanning: A CT scan is non-negotiable in stroke management. It differentiates ischemic from hemorrhagic stroke, which directly impacts treatment choices. Skipping this crucial step is unacceptable.
- Administering IV tPA outside the time window or without proper contraindication assessment: IV tPA is a powerful drug with potential risks. Administering it beyond the recommended time window or in patients with contraindications (e.g., recent major surgery, uncontrolled bleeding) can be catastrophic. Strict adherence to guidelines is paramount.
- Failing to identify and manage complications: Complications such as cerebral edema (brain swelling), seizures, or pneumonia can significantly impact outcomes. The ASP necessitates proactive monitoring and management of these complications.
- Neglecting blood pressure management: Inappropriate management of blood pressure, especially in ischemic stroke, can exacerbate brain injury. Strict adherence to established blood pressure protocols is critical.
- Ignoring the importance of dysphagia management: Difficulty swallowing (dysphagia) is common in stroke patients and necessitates specific interventions to prevent aspiration pneumonia. This aspect of post-stroke care should be part of the integrated approach of the ASP.
3. Lack of Multidisciplinary Collaboration
The ASP is not a solo endeavor; it demands a highly coordinated effort amongst multiple medical professionals:
- Poor communication between EMS, ED staff, and stroke team: Effective communication across disciplines is essential. Breakdowns in communication can lead to critical delays and errors.
- Absence of a dedicated stroke team: A dedicated stroke team, comprising neurologists, nurses, therapists, and other specialists, is crucial for efficient and effective management. A fragmented approach is detrimental.
- Insufficient involvement of allied health professionals: Speech therapists, occupational therapists, and physiotherapists play vital roles in rehabilitation and should be actively involved from the acute phase.
4. Failure to Adhere to Established Protocols and Guidelines
Deviating from established ASP protocols is a major pitfall:
- Not following established imaging protocols: Adherence to standardized imaging protocols ensures consistency and reduces delays.
- Ignoring evidence-based treatment guidelines: Treatment decisions must align with the latest evidence-based guidelines for optimal outcomes. Decisions should never be based solely on individual preference.
- Lack of ongoing education and training: Continuous education and training for healthcare professionals are crucial for maintaining proficiency and adherence to the ever-evolving ASP guidelines.
5. Inadequate Patient and Family Education
A critical aspect often overlooked is the education of patients and families:
- Insufficient pre-discharge education: Patients and their families need to understand their diagnosis, treatment plan, and potential complications to actively participate in their recovery.
- Lack of access to support services: Patients may need access to various support services, such as rehabilitation facilities, home healthcare, and support groups. This needs to be incorporated into post-discharge planning.
The Importance of Understanding the Acute Stroke Pathway
Understanding which actions are not part of the ASP is as critical as understanding what is included. Every delay, every incorrect decision, and every lapse in communication can have devastating consequences. By recognizing these pitfalls, healthcare professionals can strive for a more efficient and effective approach to stroke management, ultimately improving patient outcomes and saving lives. The ASP's effectiveness relies on a coordinated, time-sensitive, and evidence-based approach where every action must contribute to the ultimate goal: minimizing disability and maximizing recovery for stroke survivors. Continuous refinement and rigorous adherence to established protocols are key to achieving this goal. The time-sensitive nature of stroke demands meticulous adherence to the ASP, ensuring that every minute counts in the battle to preserve brain function.
Latest Posts
Latest Posts
-
Perks Of Being A Wallflower Quotes Book
Mar 06, 2025
-
Unit 6 Progress Check Mcq Ap Lang
Mar 06, 2025
-
Origin Of Species Summary By Chapter
Mar 06, 2025
-
What Are Strengths And Weaknesses Of Harrahs Gainsharing
Mar 06, 2025
-
Match Each Concept To Its Definition
Mar 06, 2025
Related Post
Thank you for visiting our website which covers about Which Action Is Not Part Of The Acute Stroke Pathway . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
