Which Biopsychosocial Need Is The Priority In The Acute Phase
Onlines
Mar 10, 2025 · 6 min read
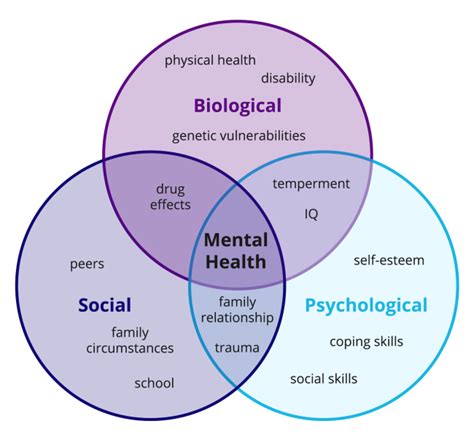
Table of Contents
Which Biopsychosocial Need is the Priority in the Acute Phase? A Holistic Approach
The acute phase of illness, injury, or crisis presents a unique challenge to healthcare providers. It's a time of intense physiological upheaval, emotional distress, and often, significant social disruption. While immediate physical needs are undeniably paramount, prioritizing just one aspect of the biopsychosocial model—biological, psychological, or social—is inadequate and potentially harmful. Effectively managing the acute phase necessitates a holistic approach that considers and balances all three dimensions simultaneously. Determining which need takes precedence in any given situation requires careful clinical judgment, informed by a thorough assessment of the individual's unique circumstances.
Understanding the Biopsychosocial Model in Acute Care
The biopsychosocial model posits that biological, psychological, and social factors are interwoven and mutually influential in health and illness. In the acute phase, this interplay becomes intensely apparent. For example:
-
Biological Factors: These are the physiological manifestations of the illness or injury, including pain, fever, inflammation, organ dysfunction, and compromised physiological reserves. Managing these factors often involves immediate medical interventions such as surgery, medication, fluid resuscitation, and pain management.
-
Psychological Factors: The acute phase triggers powerful emotional responses. Fear, anxiety, depression, denial, and even post-traumatic stress symptoms are common. These psychological factors can significantly impact the patient's ability to cope with the illness, adhere to treatment plans, and experience a positive outcome.
-
Social Factors: The acute phase significantly impacts the patient's social environment. Family dynamics, social support networks, financial resources, and access to care all play crucial roles in the patient's recovery and overall well-being. Social isolation, lack of support, and financial strain can exacerbate the already challenging situation.
Prioritizing Needs: A Case-by-Case Approach
There is no single "priority" biopsychosocial need applicable to all acute situations. The urgency and importance of each factor vary dramatically depending on the individual's presentation. However, we can outline a framework for decision-making:
1. Immediate Life-Threatening Biological Needs: The Foundation
In most acute scenarios, stabilizing immediate life-threatening biological needs takes precedence. This is the cornerstone of emergency medicine and critical care. Examples include:
- Airway management: Ensuring a patent airway is crucial, often involving intubation or other airway interventions.
- Breathing support: Providing adequate oxygenation and ventilation, which might require mechanical ventilation.
- Circulation support: Addressing circulatory issues, such as hypovolemia (low blood volume) or cardiac arrest, through fluid resuscitation, blood transfusions, and cardiac support.
- Severe pain management: Controlling excruciating pain that could further compromise physiological stability. This often involves strong analgesics.
- Hemorrhage control: Stopping severe bleeding.
These biological interventions are essential for survival and form the foundation upon which further biopsychosocial care is built. Without addressing these immediate threats, attention to psychological or social factors is futile.
2. Addressing Acute Psychological Distress: The Stabilizer
Once immediate biological threats are addressed, focusing on managing acute psychological distress becomes crucial. Untreated psychological distress can negatively influence physiological recovery and adherence to treatment. Interventions might include:
- Pain and anxiety management: Providing appropriate analgesia and anxiolytics.
- Emotional support: Offering empathy, active listening, and reassurance. This might involve family members or trained mental health professionals.
- Information and education: Providing clear, concise, and honest information about the patient's condition and treatment plan reduces anxiety associated with uncertainty.
- Early identification of PTSD risk factors: Identifying patients at high risk of developing post-traumatic stress disorder and initiating preventative measures.
- Rapid access to psychological services: If needed, facilitating referrals to psychologists or psychiatrists specializing in acute trauma or crisis intervention.
Effective management of acute psychological distress is not merely about alleviating symptoms; it also facilitates better collaboration with the healthcare team, improved adherence to treatment plans, and faster recovery.
3. Addressing Social Needs: The Long-Term Support System
Addressing social needs is crucial for long-term recovery and successful reintegration into society. This often involves:
- Family and support system involvement: Encouraging family involvement in care, respecting their roles, and providing support and information to the family.
- Social work intervention: Connecting patients and families with social workers who can assist with discharge planning, access to resources, and addressing social determinants of health.
- Financial assistance: Assessing the patient's financial situation and connecting them with resources to alleviate financial burdens that could impede recovery.
- Discharge planning: Developing a comprehensive discharge plan that addresses the patient's physical, psychological, and social needs, ensuring a safe and smooth transition from the acute care setting to home or rehabilitation.
- Community resources: Linking patients to community resources such as support groups, rehabilitation facilities, and home healthcare services.
Addressing social needs is particularly crucial for preventing readmission to the hospital and promoting a more holistic recovery process.
The Interconnectedness: A Holistic Approach
It's crucial to recognize the profound interconnectedness of these three domains. For example, untreated pain (biological) can lead to anxiety and depression (psychological), hindering engagement with social support systems. Similarly, social isolation (social) can exacerbate psychological distress and negatively impact physiological recovery. A holistic approach necessitates:
- Regular reassessment: Continuously assessing the patient's biological, psychological, and social needs throughout the acute phase to adapt the care plan as needed.
- Collaboration: Fostering effective collaboration among healthcare professionals, including physicians, nurses, social workers, psychologists, and other members of the interdisciplinary team.
- Patient-centered care: Prioritizing the patient's individual needs and preferences, respecting their autonomy, and empowering them to participate in decision-making.
- Communication: Establishing open and effective communication channels between the patient, family, and healthcare team.
Examples of Prioritization Challenges
Let's consider a few scenarios to illustrate the complexity of prioritizing biopsychosocial needs:
Scenario 1: Trauma Patient
A patient arrives after a serious car accident with multiple injuries, including a severe head injury, internal bleeding, and fractures. The immediate priority is undoubtedly the biological needs: securing the airway, controlling bleeding, and stabilizing vital signs. Once stabilized, attention shifts to managing psychological distress, addressing pain, and providing emotional support. Social needs, such as family contact and discharge planning, become more prominent after the immediate crisis is addressed.
Scenario 2: Cardiac Arrest Survivor
A patient survives cardiac arrest but experiences significant psychological trauma. While the immediate biological need (restoration of circulation) was the priority initially, the subsequent psychological needs become central. Addressing the fear, anxiety, and potentially PTSD requires specialized psychological support. Social support from family and community is also crucial for long-term recovery.
Scenario 3: Patient with Severe Depression Experiencing Acute Medical Illness
A patient with pre-existing severe depression develops pneumonia. While treating the pneumonia (biological) is critical, addressing the patient's existing psychological fragility is paramount for overall recovery. Medication management for both the pneumonia and the depression is needed, as is psychological support. Engaging social support systems is also crucial for adherence to treatment and preventing relapse.
Conclusion
Prioritizing biopsychosocial needs in the acute phase is not a linear process. It's a dynamic, iterative approach requiring continuous assessment and adaptation. While immediate life-threatening biological needs almost always take precedence initially, ignoring the psychological and social dimensions risks incomplete and potentially detrimental care. A holistic approach that values the interconnectedness of these three domains, ensures patient-centered care, and fosters collaboration among healthcare professionals is crucial for achieving optimal outcomes in the acute phase and beyond. The ultimate goal is to not only save lives but also to promote comprehensive recovery, ensuring patients are not only physically healed but also psychologically and socially supported to thrive.
Latest Posts
Latest Posts
-
Basic Communication Crossword Notes Puzzle Answers
Mar 10, 2025
-
How Do You Individualize A Patients Care Plan In Epic
Mar 10, 2025
-
Rising Action Examples In Helen Keller
Mar 10, 2025
-
A Nurse Is Preparing To Administer Esomeprazole 40 Mg
Mar 10, 2025
-
Select All The Descriptions About Art And The Sacred Realm
Mar 10, 2025
Related Post
Thank you for visiting our website which covers about Which Biopsychosocial Need Is The Priority In The Acute Phase . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
