Which Event Must Precede All Others During Tissue Repair
Onlines
Mar 16, 2025 · 6 min read
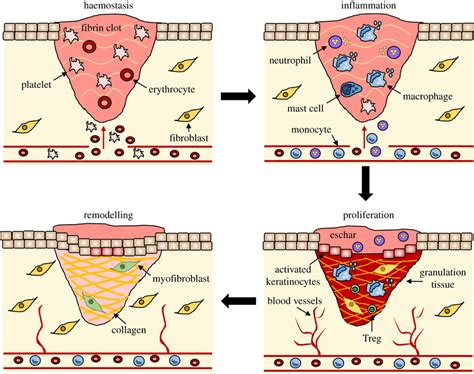
Table of Contents
Which Event Must Precede All Others During Tissue Repair?
Tissue repair, a complex and fascinating process, is crucial for our survival. From minor scrapes to significant injuries, our bodies possess an intricate mechanism to restore damaged tissue. But for this process to be effective and efficient, a specific event must occur before any other: hemostasis. Understanding why hemostasis is the foundational step in tissue repair is key to appreciating the entire process. This article will delve deep into the mechanisms of hemostasis, its crucial role in initiating tissue repair, and the cascading effects of its failure.
The Cornerstone of Repair: Hemostasis Explained
Hemostasis, simply put, is the process of stopping bleeding. It's not merely about plugging a hole; it's a highly orchestrated sequence of events designed to maintain vascular integrity and prevent excessive blood loss. Without effective hemostasis, the subsequent stages of tissue repair cannot proceed effectively, leading to complications and potentially life-threatening situations. Think of hemostasis as the foundation upon which the entire edifice of tissue repair is built. Without a strong foundation, the whole structure is at risk of collapse.
Hemostasis involves a complex interplay of vascular, platelet, and coagulation systems. These systems work together in a tightly regulated manner to achieve the crucial goal of bleeding cessation. Let's examine each component individually:
1. Vascular Spasm: The Immediate Response
The initial response to injury is vasoconstriction. Damaged blood vessels constrict, reducing blood flow to the injured site. This immediate reduction in blood flow minimizes blood loss and buys time for the other hemostatic mechanisms to kick in. This vasoconstriction is mediated by neurotransmitters, such as serotonin and norepinephrine, released from nerve endings and platelets at the site of injury. It's a rapid, reflexive response, essential for the initial control of bleeding.
2. Platelet Plug Formation: The Primary Hemostatic Plug
Following vasoconstriction, platelets play a crucial role. These tiny, anucleated cells are activated upon contact with the exposed collagen in the damaged vessel wall. This activation triggers a cascade of events, including:
- Adhesion: Platelets adhere to the exposed collagen via von Willebrand factor (vWF), a protein that acts as a bridge between platelets and collagen.
- Activation: Adherent platelets undergo shape change, becoming spiky and releasing the contents of their granules. These granules contain numerous substances that promote further platelet aggregation and vasoconstriction.
- Aggregation: Activated platelets attract and bind to each other, forming a platelet plug. This plug is a temporary seal, but it effectively reduces bleeding. The key molecule mediating platelet aggregation is ADP (adenosine diphosphate), released from activated platelets and the damaged endothelium.
This primary hemostatic plug is crucial, but it's not sufficient on its own for complete hemostasis in larger vessels. It requires the support of the coagulation cascade to form a more stable and permanent clot.
3. Coagulation Cascade: The Secondary Hemostatic Plug
The coagulation cascade is a complex series of enzymatic reactions that ultimately lead to the formation of a stable fibrin clot. This clot reinforces the platelet plug, providing a robust barrier to further blood loss. The cascade can be broadly divided into two pathways:
- Intrinsic Pathway: This pathway is activated by contact with negatively charged surfaces exposed by the injury.
- Extrinsic Pathway: This pathway is activated by tissue factor (TF), a protein released from damaged cells.
Both pathways converge at a common point, leading to the activation of thrombin. Thrombin converts soluble fibrinogen into insoluble fibrin, forming a mesh-like network that traps platelets, red blood cells, and other blood components, solidifying the clot. The fibrin clot is far more substantial and durable than the platelet plug alone, effectively sealing off the injured vessel.
Why Hemostasis Must Precede All Other Stages
The importance of hemostasis in tissue repair cannot be overstated. Its failure has profound implications, affecting every subsequent stage:
- Inflammation: If bleeding continues unchecked, inflammation becomes uncontrolled and excessive, potentially leading to tissue damage beyond the initial injury. Hemostasis limits the spread of inflammatory mediators, confining the inflammatory response to the site of injury.
- Proliferation: The formation of granulation tissue, a crucial step in the proliferative phase of tissue repair, requires a stable environment. Continuous bleeding hinders the migration and proliferation of fibroblasts and endothelial cells, delaying wound healing.
- Remodeling: The final stage of tissue repair, remodeling, involves the maturation and organization of the connective tissue. Continued bleeding interferes with the deposition and organization of collagen fibers, resulting in a weaker, less functional scar.
In essence, hemostasis creates the necessary conditions for the other stages of tissue repair to proceed effectively. Without a controlled environment, the subsequent phases will be compromised, resulting in delayed or impaired healing.
Consequences of Hemostatic Failure
The consequences of inadequate hemostasis can be severe, ranging from prolonged bleeding and hematoma formation to life-threatening hemorrhage. These consequences are particularly profound in situations involving significant trauma or injury to large blood vessels. Failure of hemostasis can also lead to:
- Infection: An open wound provides a portal for pathogens, and uncontrolled bleeding increases the risk of infection.
- Scarring: Excessive inflammation due to ongoing bleeding can lead to excessive scar tissue formation, impacting the functionality of the repaired tissue.
- Chronic wounds: Failure of hemostasis contributes significantly to the development of chronic wounds, which fail to heal within a reasonable timeframe. These wounds are often associated with significant morbidity and impaired quality of life.
Clinical Relevance: Hemostatic Disorders
Many clinical conditions can impair hemostasis, leading to bleeding complications. These include:
- Hemophilia: A group of inherited disorders characterized by a deficiency in clotting factors.
- Von Willebrand Disease: The most common inherited bleeding disorder, affecting the function of von Willebrand factor.
- Thrombocytopenia: A low platelet count, which impairs platelet plug formation.
- Liver disease: The liver plays a crucial role in the synthesis of clotting factors, and liver disease can impair coagulation.
- Use of anticoagulant medications: Medications such as warfarin and heparin are used to prevent blood clotting, but they can increase the risk of bleeding.
Understanding the mechanisms of hemostasis is crucial for the diagnosis and management of these disorders. Effective treatment strategies are aimed at restoring hemostatic balance and preventing excessive bleeding.
Conclusion: The Primacy of Hemostasis in Tissue Repair
In conclusion, hemostasis is the paramount event in tissue repair. It provides the essential foundation upon which all subsequent stages are built. Its critical role in controlling bleeding, limiting inflammation, and creating a conducive environment for tissue regeneration cannot be overemphasized. The intricate interplay of vascular, platelet, and coagulation systems demonstrates the remarkable complexity and efficiency of our body's natural healing mechanisms. Appreciating the primacy of hemostasis provides a deeper understanding of tissue repair and its clinical implications. Failure to achieve effective hemostasis inevitably compromises the healing process, underscoring its fundamental and irreplaceable role in restoring tissue integrity. Further research into the intricacies of hemostasis continues to unravel the secrets of this vital process and provide new insights for improving tissue repair and wound healing strategies.
Latest Posts
Latest Posts
-
Balzac And The Little Chinese Seamstress Summary
Mar 16, 2025
-
Summary Of Scarlet Letter Chapter 1
Mar 16, 2025
-
Summary Of Chapter 5 Of The Giver
Mar 16, 2025
-
European And American Indian First Encounters Dbq
Mar 16, 2025
-
Covey Matrix Eight Dimensions Of Wellness
Mar 16, 2025
Related Post
Thank you for visiting our website which covers about Which Event Must Precede All Others During Tissue Repair . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
