Which Of The Following Statements Is True Regarding Pain Management
Onlines
Apr 01, 2025 · 7 min read
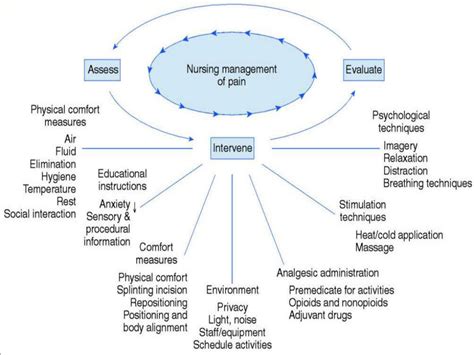
Table of Contents
Which of the Following Statements is True Regarding Pain Management? A Comprehensive Guide
Pain management is a complex and multifaceted field, encompassing a wide range of approaches and considerations. Understanding the nuances of pain, its causes, and effective management strategies is crucial for both healthcare professionals and individuals experiencing pain. This article aims to clarify common misconceptions and provide a comprehensive overview of pain management, ultimately addressing the question: which of the following statements is true regarding pain management? While we won't present a multiple-choice question directly, we will explore several common assertions about pain management, validating or refuting them with evidence-based information.
Debunking Myths and Unveiling Truths in Pain Management
Many misconceptions surround pain management, often leading to ineffective strategies and unnecessary suffering. Let's delve into some common statements and dissect their validity:
Statement 1: "Pain is purely a physical sensation."
False. While pain certainly has a physical component, involving nociceptors (pain receptors) and neural pathways, it's inaccurate to consider it solely a physical sensation. Pain is a complex biopsychosocial phenomenon. This means it's influenced by:
-
Biological factors: These include the intensity of the noxious stimulus, the individual's genetics, and the presence of underlying medical conditions. Nerve damage, inflammation, and tissue injury all contribute significantly.
-
Psychological factors: Emotional states like anxiety, depression, and stress can significantly amplify pain perception. Past experiences, coping mechanisms, and beliefs about pain also play a crucial role. Catastrophizing (exaggerating the threat of pain) can exacerbate the experience.
-
Social factors: Social support, cultural norms, and access to healthcare significantly influence how pain is experienced and managed. Social isolation and lack of support can worsen pain perception.
The truth: Pain is a subjective experience shaped by the intricate interplay of biological, psychological, and social factors. Effective pain management requires a holistic approach, addressing all these dimensions.
Statement 2: "Opioids are always the best treatment for chronic pain."
False. This is a dangerously misleading statement. While opioids can be effective in managing acute, severe pain (like post-surgical pain), their long-term use for chronic pain is associated with significant risks, including:
-
Physical dependence and addiction: Chronic opioid use can lead to dependence, necessitating escalating doses to achieve the same pain relief, and ultimately, addiction.
-
Tolerance: The body adapts to opioids over time, requiring higher doses for the same effect.
-
Side effects: Opioids can cause constipation, nausea, drowsiness, respiratory depression, and other serious side effects.
-
Overdose risk: Accidental overdose is a significant concern, particularly with combinations of opioids and other sedatives.
The truth: Opioids should be considered only as a last resort for chronic pain management, and only under strict medical supervision. A multi-modal approach that combines non-pharmacological and pharmacological strategies is generally preferred for chronic pain. This might include physical therapy, cognitive-behavioral therapy (CBT), lifestyle modifications, and other medications like NSAIDs or antidepressants.
Statement 3: "Pain is a necessary consequence of aging."
False. While some age-related changes (like osteoarthritis) may cause pain, pain is not an inevitable part of aging. Many older adults live pain-free. The increase in pain incidence with age is often related to accumulated injuries, chronic conditions, and decreased mobility, rather than aging itself.
The truth: Pain in older adults warrants a thorough evaluation to identify and address underlying causes, rather than accepting it as a normal part of aging. Effective management strategies can significantly improve quality of life for older individuals. These strategies need to account for potential polypharmacy and age-related physiological changes.
Statement 4: "Ignoring pain is the best way to manage it."
False. Ignoring pain is not only ineffective but also potentially harmful. Persistent pain can lead to:
-
Physical disability: Chronic pain can limit mobility and function, leading to reduced independence.
-
Mental health problems: Chronic pain is strongly linked to depression, anxiety, and other mental health disorders.
-
Sleep disturbances: Pain can severely disrupt sleep, resulting in fatigue and impaired cognitive function.
-
Cardiovascular problems: Chronic pain has been linked to increased risk of cardiovascular diseases.
The truth: Addressing pain promptly and effectively is crucial for preventing these negative consequences. Early intervention and proactive pain management strategies are essential for maintaining physical and mental well-being.
Statement 5: "There's nothing that can be done for chronic pain."
False. While chronic pain can be challenging to manage, there are many effective treatments available. The key is finding the right combination of approaches tailored to the individual's specific needs. This may involve a combination of:
-
Pharmacological treatments: These include various analgesics (pain relievers), antidepressants, anticonvulsants, and other medications, each with its own mechanism of action and potential side effects.
-
Non-pharmacological treatments: These include physical therapy, occupational therapy, CBT, mindfulness-based stress reduction (MBSR), acupuncture, massage therapy, and other modalities. These approaches aim to improve function, reduce pain perception, and enhance coping strategies.
-
Interventional procedures: In some cases, interventional procedures like nerve blocks or spinal cord stimulation may be considered to provide targeted pain relief.
-
Lifestyle modifications: Changes in diet, exercise, and sleep habits can significantly impact pain levels.
The truth: Chronic pain management is a journey, not a destination. A collaborative approach involving the patient, healthcare providers, and potentially family members, is essential for developing a personalized treatment plan that aims for optimal pain relief and improved quality of life.
Comprehensive Pain Management Strategies: A Holistic Approach
Effective pain management necessitates a multi-pronged strategy that considers the individual's unique circumstances and pain characteristics. Key components of a holistic approach include:
1. Accurate Diagnosis and Assessment:
A thorough evaluation is paramount to identify the underlying cause of pain. This involves a detailed medical history, physical examination, and potentially imaging studies (X-rays, MRI, CT scans). Pain assessment tools, such as pain scales (visual analog scale, numeric rating scale) and questionnaires, help quantify pain intensity and impact on daily life.
2. Pharmacological Interventions:
Various medications are used to manage pain, ranging from over-the-counter analgesics (like acetaminophen and ibuprofen) to prescription opioids, antidepressants, and anticonvulsants. The choice of medication depends on the type and severity of pain, the individual's medical history, and potential side effects.
3. Non-Pharmacological Interventions:
These play a vital role in chronic pain management. Examples include:
-
Physical Therapy: Improves mobility, strengthens muscles, and improves function.
-
Occupational Therapy: Adapts daily activities to reduce strain and pain.
-
Cognitive Behavioral Therapy (CBT): Helps individuals develop coping strategies to manage pain and its emotional impact. This includes techniques for reframing thoughts and behaviors associated with pain.
-
Mindfulness-Based Stress Reduction (MBSR): Teaches mindfulness techniques to reduce stress and improve pain tolerance.
-
Acupuncture and other complementary therapies: These may provide additional relief for some individuals, although scientific evidence for their efficacy varies.
4. Lifestyle Modifications:
Lifestyle adjustments can significantly impact pain management. These include:
-
Regular Exercise: Improves physical function, reduces stiffness, and boosts mood. Gentle, low-impact exercises are often recommended for those with chronic pain.
-
Healthy Diet: Provides the body with the nutrients needed for healing and reduces inflammation.
-
Adequate Sleep: Promotes healing and reduces stress. Addressing sleep disturbances is crucial for effective pain management.
-
Stress Management Techniques: Stress can exacerbate pain. Techniques like yoga, meditation, deep breathing exercises can help reduce stress levels.
5. Interventional Procedures:
These are considered when other treatments have failed to provide adequate pain relief. Examples include:
-
Nerve Blocks: Injections that temporarily block pain signals.
-
Spinal Cord Stimulation: Implants electrodes near the spinal cord to modulate pain signals.
-
Radiofrequency Ablation: Uses heat or radio waves to destroy pain-causing nerves.
Conclusion: A Personalized Approach to Effective Pain Management
The question, "Which of the following statements is true regarding pain management?" doesn't have a single, simple answer. The truth is far more nuanced. Effective pain management is a personalized journey requiring a holistic approach that addresses the biological, psychological, and social factors contributing to an individual's pain experience. A collaborative effort between the patient, healthcare providers, and potentially family members is crucial for developing a tailored plan that combines pharmacological and non-pharmacological strategies, lifestyle modifications, and potentially interventional procedures. Misconceptions about pain management can lead to ineffective strategies and unnecessary suffering. Understanding the complexity of pain and the range of available treatments is crucial for improving the lives of those affected by chronic and acute pain. The key is to seek professional help, engage in open communication with healthcare providers, and actively participate in developing a personalized management plan. Remember, pain is a complex issue that deserves a comprehensive and tailored approach.
Latest Posts
Latest Posts
-
Escoge La Opcion Que Mejor Resume El Cortometraje
Apr 02, 2025
-
Which Statement Best Explains The Relationship Between Diet And Osteoporosis
Apr 02, 2025
-
Dod Personnel Who Suspect A Coworker Of Possible Espionage
Apr 02, 2025
-
True Or False Behavior Is A Form Of Communication
Apr 02, 2025
-
Main Characters In Brave New World
Apr 02, 2025
Related Post
Thank you for visiting our website which covers about Which Of The Following Statements Is True Regarding Pain Management . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
