Which Patient Data Signals Improper Placement Of The Endotracheal Tube
Onlines
Apr 07, 2025 · 5 min read
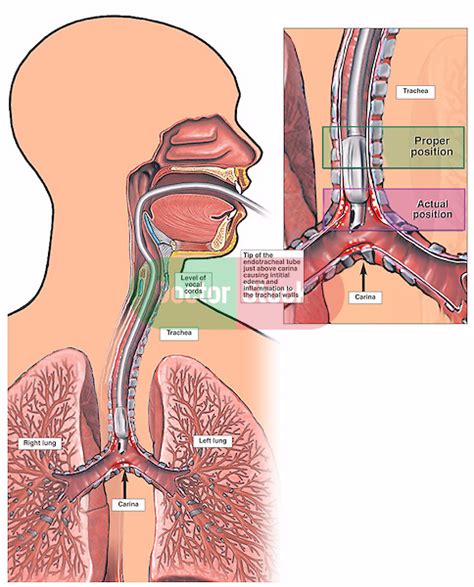
Table of Contents
Which Patient Data Signals Improper Placement of the Endotracheal Tube?
Endotracheal intubation, a critical procedure in emergency medicine and critical care, involves inserting a tube into the trachea to secure an airway and facilitate mechanical ventilation. While a life-saving technique, improper placement can lead to serious complications, including hypoxia, lung injury, and even death. Therefore, meticulous attention to detail and the careful interpretation of patient data are crucial for confirming correct endotracheal tube (ETT) placement. This article will explore the various patient data signals that indicate improper ETT placement, emphasizing the importance of proactive monitoring and prompt corrective action.
I. Immediate Post-Intubation Assessment: The Crucial First Steps
The immediate period following intubation is the most critical for detecting misplaced tubes. Several assessments should be performed immediately to verify proper placement:
A. Auscultation: Listening for Breath Sounds
Auscultation, the act of listening to the lungs with a stethoscope, is a cornerstone of post-intubation assessment. Bilateral breath sounds, indicating air entry into both lungs, are expected following successful intubation. However, the absence of breath sounds, unilateral breath sounds, or the presence of breath sounds over the epigastrium (stomach) strongly suggests misplacement.
Absence of breath sounds: This points towards esophageal intubation or a severely obstructed airway. Unilateral breath sounds: This suggests the ETT may be in the mainstem bronchus, obstructing ventilation to one lung. Epigastric breath sounds: This indicates that the ETT is in the esophagus, with air entering the stomach.
B. Chest Rise and Fall: Visual Confirmation
Observing symmetrical chest rise and fall is a fundamental visual assessment. Asymmetrical chest movement, where one side rises more than the other, points towards mainstem intubation or other airway issues. The absence of chest rise indicates a critical problem requiring immediate intervention.
C. End-Tidal CO2 Detection (Capnography): The Gold Standard
Capnography, measuring the concentration of carbon dioxide (CO2) in exhaled breath, is considered the gold standard for confirming proper ETT placement. A waveform showing a detectable CO2 level (typically 35-45 mmHg) strongly supports tracheal intubation. Absence of a CO2 waveform indicates potential esophageal intubation or severe airway obstruction. However, it's essential to note that some factors can affect capnography readings (e.g., poor perfusion, cardiac arrest).
Absence of CO2 waveform: This is a major red flag indicating potential misplacement, often requiring immediate re-assessment and intervention. Low or fluctuating CO2 levels: While a waveform is present, abnormally low or fluctuating CO2 levels might suggest inadequate ventilation or other underlying issues.
D. Pulse Oximetry: Monitoring Oxygen Saturation
While pulse oximetry doesn't directly confirm ETT placement, it's crucial for monitoring oxygen saturation (SpO2). A persistently low SpO2 despite ventilation strongly suggests a problem with oxygen delivery, potentially related to improper ETT placement. However, a normal SpO2 doesn't automatically confirm correct placement; it's only one piece of the puzzle.
II. Ongoing Monitoring: Continuous Vigilance After Intubation
Even after initial confirmation, continuous monitoring is critical to detect potential problems.
A. Continuous Capnography: Maintaining Vigilance
Continuous capnography provides a real-time graphical representation of ETCO2. Sudden changes in waveform or ETCO2 levels should trigger immediate investigation.
B. Arterial Blood Gases (ABGs): A More Detailed Picture
ABGs provide a more detailed analysis of blood gases, including pH, PaO2 (partial pressure of oxygen), PaCO2 (partial pressure of carbon dioxide), and bicarbonate. Abnormal ABGs can indicate ventilation-perfusion mismatch, a common complication of improper ETT placement. Hypoxemia (low PaO2) and hypercapnia (high PaCO2) are major warnings signs.
C. Chest X-Ray: Definitive Confirmation of Position
A chest X-ray is essential for definitive confirmation of ETT placement. It visually confirms the location of the ETT tip within the trachea and helps identify potential complications like pneumothorax or mainstem intubation. This should be performed shortly after intubation and repeated if there's any clinical suspicion of misplacement. The radiograph should clearly show the ETT tip approximately 2-6 cm above the carina (the point where the trachea branches into the two main bronchi).
D. Clinical Assessment: Ongoing Observation
Continuous clinical observation is vital. Signs like increased work of breathing, cyanosis (bluish discoloration of the skin and mucous membranes), decreased breath sounds, or asymmetrical chest movement all warrant reassessment of ETT position. Changes in vital signs, including heart rate, blood pressure, and respiratory rate, may also indicate complications.
III. Specific Signs of Improper ETT Placement
Certain clinical findings strongly suggest specific types of ETT misplacement:
A. Esophageal Intubation: Air in the Stomach
Esophageal intubation, where the ETT is placed in the esophagus instead of the trachea, is a critical error. Key indicators include:
- Absence of breath sounds.
- Absence of end-tidal CO2.
- Presence of breath sounds over the epigastrium.
- Poor oxygen saturation (SpO2).
- Distended abdomen (due to air insufflation).
B. Mainstem Intubation: Ventilation to One Lung
Mainstem intubation, where the ETT is wedged into one of the main bronchi, typically the right, leads to ventilation of only one lung. This causes serious hypoxemia in the non-ventilated lung. Signs include:
- Unilateral breath sounds.
- Asymmetrical chest rise and fall.
- Hypoxemia (low PaO2).
- Hypercapnia (high PaCO2).
C. Other Potential Complications: Beyond Misplacement
Improper ETT placement can contribute to other complications such as:
- Pneumothorax: Air leakage into the pleural space, potentially causing lung collapse. Signs include decreased breath sounds, asymmetrical chest movement, and respiratory distress.
- Tracheal or esophageal perforation: These are rare but potentially life-threatening complications.
- Tracheal stenosis: Narrowing of the trachea due to prolonged intubation or trauma.
- Infection: Risk of infection is higher with prolonged intubation.
IV. Importance of Teamwork and Proper Training
Confirming proper ETT placement is not the responsibility of a single individual. A team-based approach involving the anesthesiologist, intensivist, respiratory therapist, and nurses is essential. All team members must be proficient in assessing and interpreting the various signals discussed above. Regular training and simulation exercises are critical for maintaining competency in this crucial procedure.
V. Conclusion: A Multifaceted Approach to Safety
Ensuring proper ETT placement requires a multifaceted approach combining immediate post-intubation assessment, continuous monitoring, and diligent interpretation of patient data. By understanding and actively looking for the warning signs outlined above, healthcare professionals can significantly reduce the risk of complications associated with improper ETT placement. Remember, the timely recognition and correction of improper ETT placement can be life-saving. Proactive vigilance and adherence to established protocols are paramount in ensuring patient safety. Continuous learning and the integration of advanced technologies remain crucial for enhancing the safety and effectiveness of endotracheal intubation.
Latest Posts
Latest Posts
-
Which Action Is Most Likely To Positively Impact His Survival
Apr 09, 2025
-
Impressions Of An Indian Childhood Summary
Apr 09, 2025
-
Twenty Thousand Leagues Under The Sea Quotes
Apr 09, 2025
-
1 4 Skills Practice Angle Measure
Apr 09, 2025
-
Activity 3 1 Linear Measurement With Metric Units
Apr 09, 2025
Related Post
Thank you for visiting our website which covers about Which Patient Data Signals Improper Placement Of The Endotracheal Tube . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.