Which Three Statements About Dialysis Are True
Onlines
Mar 19, 2025 · 5 min read
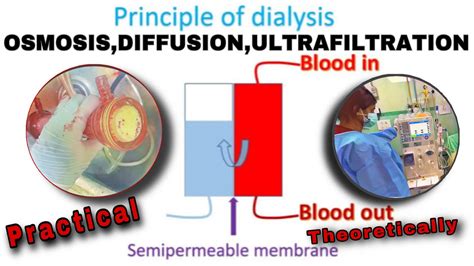
Table of Contents
Which Three Statements About Dialysis Are True? A Comprehensive Guide
Dialysis, a life-sustaining treatment for individuals with kidney failure, is a complex process with many facets. Understanding dialysis is crucial for patients, families, and healthcare professionals alike. While countless statements can be made about dialysis, let's focus on identifying three accurate assertions from a broader range of possibilities. This article will delve into the specifics of dialysis, clarifying common misconceptions and providing a comprehensive overview of this vital medical intervention. We will explore different types of dialysis, their functionalities, and the overall impact they have on patients' lives.
Understanding Kidney Failure and the Need for Dialysis
Before diving into specific truths about dialysis, it's essential to understand the underlying condition it addresses: kidney failure, also known as end-stage renal disease (ESRD). Healthy kidneys filter waste products, excess fluid, and electrolytes from the blood, maintaining the body's delicate chemical balance. When kidneys fail, these vital functions are compromised, leading to a buildup of toxins in the bloodstream and a disruption of essential bodily processes. This can result in a range of serious symptoms, including:
- Fatigue and weakness: The accumulation of toxins leads to overall lethargy and reduced energy levels.
- Swelling (edema): Fluid retention causes swelling in the legs, ankles, and other parts of the body.
- Shortness of breath: Fluid buildup can put pressure on the lungs.
- Nausea and vomiting: The body's attempt to expel toxins can lead to gastrointestinal distress.
- Changes in urination: Reduced urine output or complete absence of urine is a hallmark of kidney failure.
- Itching: A buildup of toxins can cause intense itching.
- High blood pressure: Kidney failure often contributes to uncontrolled hypertension.
- Bone pain: Kidney disease affects calcium and phosphorus metabolism, leading to bone weakening.
When conservative treatments such as medication and dietary changes are insufficient, dialysis becomes a necessary intervention to maintain life and alleviate the symptoms of kidney failure. Dialysis artificially performs the filtering function of the kidneys, removing waste products and excess fluid from the blood.
Three True Statements About Dialysis
Now, let's address three crucial truths about dialysis:
1. Dialysis is a life-sustaining treatment, but it doesn't cure kidney failure.
This is a fundamental understanding that many individuals need to grasp. Dialysis, while essential for survival in cases of ESRD, doesn't repair or replace the damaged kidneys. It acts as a temporary substitute, performing the necessary filtration functions until a kidney transplant becomes possible, or as a long-term solution when a transplant isn't feasible. Patients on dialysis must undergo regular treatments for the remainder of their lives unless they receive a successful kidney transplant.
2. There are two primary types of dialysis: hemodialysis and peritoneal dialysis.
Hemodialysis and peritoneal dialysis represent the two main approaches to dialysis, each with its own mechanisms and advantages/disadvantages.
Hemodialysis: This involves using an artificial kidney machine (dialyzer) to filter the blood externally. A needle is inserted into a surgically created access point (usually a fistula or graft) in the arm or leg, and blood is pumped through the dialyzer, where waste products are removed. Cleansed blood is then returned to the body. Hemodialysis sessions typically last several hours, three times a week at a dialysis center.
Peritoneal dialysis: This utilizes the patient's own peritoneal membrane (the lining of the abdominal cavity) as a natural filter. A catheter is surgically implanted into the abdomen, and a dialysis solution is infused into the peritoneal cavity. The solution absorbs waste products and excess fluid from the blood through the peritoneal membrane. After a dwell time (typically several hours), the solution is drained and discarded. Peritoneal dialysis can be performed at home, offering greater flexibility. There are two main types: continuous ambulatory peritoneal dialysis (CAPD), where patients exchange the solution several times a day manually, and continuous cycler-assisted peritoneal dialysis (CCPD), where an automated machine performs the exchanges overnight.
3. Dialysis significantly improves the quality of life for patients with kidney failure, but it also carries potential risks and side effects.
While dialysis is crucial for survival, it's important to acknowledge that it's not without challenges. Many patients experience improved health and a better quality of life with dialysis, as it addresses the symptoms of kidney failure. However, dialysis carries potential complications, including:
- Infection: The access site for hemodialysis or the catheter used in peritoneal dialysis can be vulnerable to infections.
- Muscle cramps: Electrolyte imbalances during dialysis can lead to painful muscle cramps.
- Low blood pressure (hypotension): Rapid fluid removal during dialysis can cause a drop in blood pressure.
- Nausea and vomiting: Dialysis can sometimes trigger gastrointestinal distress.
- Bleeding: Problems with the access site can lead to bleeding.
- Anemia: Kidney failure and dialysis can lead to a reduction in red blood cells.
- Bone disease: Dialysis can affect calcium and phosphorus metabolism, contributing to bone problems.
- Cardiovascular disease: Patients undergoing dialysis have an increased risk of cardiovascular problems.
Managing these risks and side effects requires close monitoring by healthcare professionals and adherence to the prescribed treatment plan. The success of dialysis hinges not only on the treatment itself but also on the patient's overall health, adherence to dietary restrictions, and engagement with their medical team.
Further Considerations and Conclusion
This article has explored three key truths about dialysis, clarifying the nature of this life-sustaining treatment. Remember that dialysis is a complex medical intervention, and individual experiences vary significantly. The choice between hemodialysis and peritoneal dialysis depends on several factors, including the patient's overall health, lifestyle, and preferences. Open communication between the patient, their nephrologist (kidney specialist), and other healthcare providers is essential to ensure the best possible outcome. Regular monitoring, adherence to medical advice, and a proactive approach to managing potential side effects are crucial for maintaining health and well-being during dialysis. The information provided here is for informational purposes only and does not constitute medical advice. Always consult with a qualified healthcare professional for diagnosis and treatment of any medical condition. Further research and consultation with experts are encouraged for a deeper understanding of this complex field. Remember to stay informed and actively participate in your healthcare journey to make informed decisions about your dialysis treatment. The goal is to improve quality of life and manage the challenges of kidney failure effectively.
Latest Posts
Latest Posts
-
Character List Of Catcher In The Rye
Mar 19, 2025
-
Pedro Y Natalia No Nos Dan Las Gracias
Mar 19, 2025
-
The Epic Periodic Table Scavenger Hunt
Mar 19, 2025
-
A Health Facility Using Cloud Storage For Data Backup Is
Mar 19, 2025
-
Chapter 8 Summary Of Animal Farm
Mar 19, 2025
Related Post
Thank you for visiting our website which covers about Which Three Statements About Dialysis Are True . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
