A Provider Calls Asking Why A Claim Was Denied
Onlines
Mar 25, 2025 · 6 min read
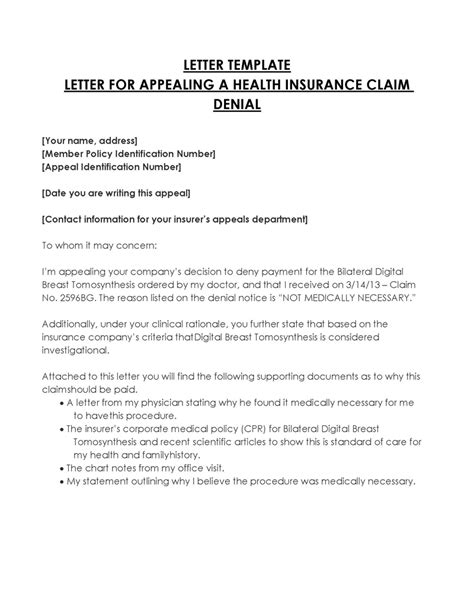
Table of Contents
A Provider Calls Asking Why a Claim Was Denied: A Comprehensive Guide
Dealing with denied claims is a frustrating but unfortunately common experience for healthcare providers. When a payer denies a claim, it's crucial to understand the reason for the denial to prevent future issues and ensure timely reimbursement. This article provides a comprehensive guide to handling provider calls regarding denied claims, covering everything from understanding common denial reasons to developing effective strategies for appeal.
Understanding Claim Denials: The First Step
Before diving into handling provider calls, it's vital to grasp the various reasons why claims might be denied. Denials fall into several broad categories:
1. Coding Errors:
- Incorrect Codes: This is a major cause of claim denials. Using the wrong Current Procedural Terminology (CPT) codes, International Classification of Diseases (ICD) codes, or Healthcare Common Procedure Coding System (HCPCS) codes can lead to immediate rejection. Even minor discrepancies can trigger a denial. Double-checking codes against the patient's medical record and the payer's guidelines is crucial.
- Missing Codes: Failing to include necessary codes, especially those related to modifiers or diagnoses, can result in denial. Ensure all relevant codes are included and correctly sequenced.
- Unbundling/Bundling Errors: Unbundling (billing separately for services that should be bundled) or bundling (billing multiple services as one) can lead to denials. Understanding payer-specific bundling rules is essential.
2. Eligibility and Patient Information Issues:
- Incorrect Patient Information: Errors in the patient's name, date of birth, address, or insurance information are frequent causes of denial. Verifying patient information against their identification documents and insurance card is critical before submitting the claim.
- Lack of Authorization: Many procedures require prior authorization from the payer. Failure to obtain authorization before providing the service will almost certainly result in a claim denial.
- Benefit Exhaustion: The patient may have used up their benefits for the year or reached their out-of-pocket maximum. Confirm the patient's eligibility and remaining benefits before providing services.
- Incorrect Insurance Information: This includes using an outdated or incorrect insurance plan code or group number. Regularly verify and update patient insurance information.
3. Medical Necessity Issues:
- Lack of Documentation: Insufficient medical documentation to support the services provided is a common reason for denial. Ensure comprehensive and detailed documentation supports the medical necessity of all procedures and services.
- Non-Covered Services: The payer might not cover the specific service provided. Review the payer's list of covered services before providing the service.
- Lack of Supporting Evidence: The payer might require additional information, such as progress notes or consultation reports, to justify the medical necessity of the services rendered.
4. Technical Errors:
- Incorrect Billing Address: Using the wrong billing address for the provider's practice can delay or prevent claim processing.
- Incomplete Claim Form: Missing information on the claim form can result in rejection. Carefully review the form before submission.
- Filing Deadline: Submitting the claim after the payer's allowed timeframe will lead to denial. Adhere strictly to deadlines.
Handling Provider Calls Regarding Denied Claims: A Step-by-Step Approach
When a provider calls inquiring about a denied claim, a systematic approach is necessary:
1. Gather Information:
- Obtain the Claim Number: This is crucial for quickly accessing the claim's details within your system.
- Identify the Specific Denial Reason: The payer's denial letter should clearly state the reason for the rejection. If not, you may need to access the payer's online portal or contact them directly.
- Review the Patient's Medical Record: Verify the accuracy of the codes, dates of service, and other information included in the claim.
- Gather Supporting Documentation: This could include progress notes, consultation reports, or other documents that support the medical necessity of the services.
2. Analyze the Denial Reason:
Once you've gathered the necessary information, carefully analyze the specific reason for the denial. This analysis will guide your response to the provider and determine the appropriate course of action. Different denial reasons require different approaches:
- Coding Errors: Correct the codes and resubmit the claim.
- Eligibility Issues: Verify the patient's eligibility and benefits before resubmission. If the patient's coverage has ended, inform the provider and discuss alternative payment options.
- Medical Necessity Issues: Gather additional supporting documentation and address the payer's concerns in a formal appeal.
- Technical Errors: Correct the errors on the claim form and resubmit it.
3. Communicate Effectively with the Provider:
- Be Empathetic and Understanding: Acknowledge the provider's frustration and assure them that you will investigate the issue thoroughly.
- Provide Clear and Concise Explanations: Explain the reason for the denial in simple, non-technical terms. Avoid medical jargon.
- Offer Solutions: Outline the steps you'll take to resolve the issue, such as correcting codes, resubmitting the claim, or filing an appeal.
- Set Realistic Expectations: Inform the provider of the timeline for resolving the issue.
4. Resubmit the Claim or File an Appeal:
- Resubmission: For simple errors like coding issues or technical errors, resubmitting the corrected claim is usually sufficient.
- Appeal: For denials related to medical necessity, you will need to file a formal appeal with the payer. This usually involves submitting additional documentation and providing a detailed explanation of why the claim should be approved.
Preventing Future Denials: Proactive Measures
Proactive measures are crucial in minimizing claim denials:
- Regularly Update Provider Information: Ensure all provider information, such as addresses and tax IDs, is up to date in your billing system.
- Implement Robust Coding Protocols: Establish clear guidelines and training for staff regarding accurate coding practices.
- Implement a Pre-Authorization Process: Develop a streamlined process for obtaining prior authorizations for procedures requiring them.
- Thorough Documentation: Train staff to maintain comprehensive and accurate medical documentation supporting all services provided.
- Regularly Review Payer Guidelines: Stay updated on payer-specific rules and regulations to prevent non-compliance.
- Utilize Claim Scrubbing Software: Invest in claim scrubbing software to identify and correct potential errors before submitting claims.
The Importance of Strong Provider Relationships
Effectively managing denied claims and communicating with providers is vital for maintaining strong, positive relationships. Open communication, timely responses, and a proactive approach will foster trust and contribute to a smoother billing process. Investing in training for staff who handle provider inquiries will improve their ability to provide clear, accurate information and resolve issues effectively.
Conclusion
Handling provider calls regarding denied claims requires a methodical approach. By understanding common denial reasons, implementing effective communication strategies, and taking proactive measures, healthcare providers can significantly reduce the frequency of denials and ensure timely reimbursements. Building a strong relationship with providers through clear and empathetic communication further strengthens the overall revenue cycle management process. Remember, preventing denials is always more cost-effective and efficient than handling appeals.
Latest Posts
Latest Posts
-
How Many Chapters In The Things They Carried
Mar 26, 2025
-
All Of The Following Are Ways To Promote The Sharing
Mar 26, 2025
-
Select All Correct Statements On Whistleblowing
Mar 26, 2025
-
Anticipating Potential Provider Prescriptions System Disorder
Mar 26, 2025
-
Quotes From The Letter From Birmingham Jail
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about A Provider Calls Asking Why A Claim Was Denied . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
