An Index Of Suspicion Is Most Accurately Defined As
Onlines
Mar 27, 2025 · 7 min read
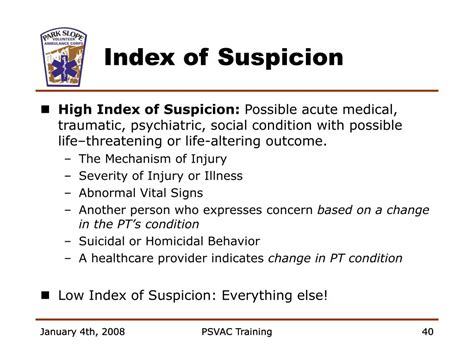
Table of Contents
An Index of Suspicion: A Deep Dive into Defining and Applying Clinical Reasoning
The phrase "index of suspicion" is a cornerstone of effective medical practice and clinical reasoning. It's a concept that transcends specific diagnoses and applies across various medical fields. Yet, despite its importance, a clear, concise, and universally accepted definition remains elusive. This article aims to provide a comprehensive understanding of the index of suspicion, exploring its accurate definition, the factors that influence it, its role in diagnostic decision-making, and its crucial impact on patient care.
Defining the Index of Suspicion: Beyond a Simple Definition
At its core, the index of suspicion refers to the clinician's subjective assessment of the likelihood that a specific condition or disease is present in a patient, based on the available evidence. It's not a rigid, quantifiable measure, but rather a dynamic, evolving judgment that informs the diagnostic and treatment process. It's more than just a hunch; it's a reasoned consideration of multiple factors, leading to a clinical judgment about the probability of a specific diagnosis.
It's crucial to differentiate the index of suspicion from other related concepts like:
-
Differential Diagnosis: This is a list of possible diagnoses based on the patient's symptoms and findings. The index of suspicion helps prioritize the differential diagnosis, focusing investigations and treatment on the most likely possibilities.
-
Clinical Probability: While related, clinical probability uses statistical data and established risk factors to estimate the likelihood of a disease. The index of suspicion integrates this information but also incorporates the clinician's experience, intuition, and the unique context of the individual patient.
-
Pre-test probability: This represents the likelihood of a condition before any diagnostic tests are performed. The index of suspicion influences the selection of tests, as it dictates which conditions warrant further investigation.
Factors Influencing the Index of Suspicion
Several key factors contribute to a clinician's index of suspicion:
1. The Patient's Presenting Complaint:
The initial symptoms and chief complaints are fundamental. A patient presenting with severe chest pain and shortness of breath will trigger a much higher index of suspicion for acute myocardial infarction (heart attack) compared to a patient with mild, intermittent indigestion. The specificity and sensitivity of the presenting symptoms play a vital role.
2. The Patient's Medical History:
Pre-existing conditions and family history significantly impact the index of suspicion. A patient with a history of heart disease presenting with chest pain will have a much higher index of suspicion for cardiac issues than a previously healthy individual. Similarly, a family history of a particular genetic disorder will raise the index of suspicion for that disorder in subsequent generations.
3. Physical Examination Findings:
Objective findings from the physical examination are crucial. Vital signs (e.g., elevated heart rate, low blood pressure), abnormal auscultation findings (e.g., heart murmurs, crackles in the lungs), and palpation findings (e.g., abdominal tenderness) all contribute to refining the index of suspicion.
4. Results of Investigations:
Laboratory tests (e.g., blood tests, urine tests), imaging studies (e.g., X-rays, CT scans, MRIs), and other diagnostic procedures provide objective data that either reinforce or challenge the initial index of suspicion. An abnormal blood test result, for instance, might significantly elevate the index of suspicion for a particular condition.
5. Epidemiological Factors:
The prevalence of certain diseases within a specific geographic area or population group influences the index of suspicion. For example, the prevalence of Lyme disease in tick-infested regions dictates a higher index of suspicion for Lyme disease in individuals with compatible symptoms who reside in those areas.
6. Clinician's Experience and Expertise:
A seasoned clinician's experience and expertise significantly influence their index of suspicion. Years of practice allow clinicians to recognize subtle patterns and nuances that might be missed by less experienced practitioners. This experience-based intuition plays a critical role, especially in cases with atypical presentations.
7. Availability of Resources:
The availability of diagnostic testing and treatment options also plays a role. In settings with limited resources, the index of suspicion might need to be adjusted based on the availability of tests and treatments.
The Index of Suspicion in Action: Case Examples
Let's consider a few hypothetical scenarios to illustrate the practical application of the index of suspicion:
Scenario 1: A 65-year-old male presents to the emergency department with sudden onset of severe chest pain radiating to his left arm. He is diaphoretic (sweaty) and short of breath. The clinician's index of suspicion for an acute myocardial infarction (heart attack) would be extremely high given the classic presentation. Immediate investigations, such as an electrocardiogram (ECG) and cardiac enzyme tests, would be prioritized.
Scenario 2: A 25-year-old female presents with a gradual onset of fatigue and joint pain. The initial index of suspicion might be lower for a serious condition, but if the symptoms persist and the physical examination reveals joint swelling and inflammation, the index of suspicion for an autoimmune disease like rheumatoid arthritis might increase. Further investigations, including blood tests, would be warranted.
Scenario 3: A 10-year-old child presents with a fever, cough, and runny nose. The initial index of suspicion might be for a common viral upper respiratory infection. However, if the child develops difficulty breathing or a worsening cough, the index of suspicion for pneumonia or other more serious respiratory infections would increase.
The Pitfalls of an Inadequate or Biased Index of Suspicion
An inadequate or biased index of suspicion can lead to significant consequences:
-
Delayed Diagnosis: A low index of suspicion for a serious condition can delay diagnosis and treatment, leading to worse outcomes. This is particularly concerning for time-sensitive conditions like stroke or sepsis.
-
Unnecessary Investigations: An excessively high index of suspicion can lead to ordering numerous unnecessary investigations, increasing healthcare costs and potentially exposing the patient to unnecessary risks.
-
Diagnostic Error: A biased index of suspicion, influenced by factors like age, race, or gender, can lead to diagnostic errors and disparities in healthcare.
-
Missed Diagnosis: Failure to consider rare or unusual conditions can lead to a missed diagnosis, with potentially devastating consequences.
Enhancing the Index of Suspicion: Strategies for Improvement
Improving the accuracy and effectiveness of the index of suspicion requires continuous learning and self-reflection:
-
Staying Updated: Keeping abreast of the latest medical research and guidelines is essential to maintain a current and accurate index of suspicion.
-
Critical Appraisal of Evidence: Clinicians must critically appraise the available evidence, considering the strengths and limitations of diagnostic tests and the potential for biases.
-
Collaborative Approach: Seeking second opinions and engaging in interdisciplinary consultations can help refine the index of suspicion and reduce diagnostic errors.
-
Reflection and Self-Assessment: Regular reflection on past cases, identifying instances where the index of suspicion was accurate or inaccurate, helps improve future clinical judgments.
-
Debiasing Strategies: Implementing strategies to mitigate biases, such as using checklists and decision support tools, can improve the accuracy of the index of suspicion.
Conclusion: The Index of Suspicion – A Dynamic Tool for Effective Clinical Practice
The index of suspicion is not merely a clinical skill; it's a critical component of effective clinical reasoning and patient care. It's a dynamic process influenced by a multitude of factors, requiring clinicians to integrate objective data with their experience, intuition, and a thorough understanding of the patient's individual context. While there's no single, universally applicable formula for calculating the index of suspicion, a conscientious and deliberate approach to this concept is essential for accurate diagnosis, timely treatment, and ultimately, improved patient outcomes. Continuous learning, critical self-reflection, and a commitment to reducing biases are crucial for honing this crucial clinical skill. By mastering the art of the index of suspicion, clinicians can significantly enhance their diagnostic accuracy and provide the best possible care for their patients.
Latest Posts
Latest Posts
-
Edulastic Formative And Summative Assessments Made Easy Answer Key
Mar 30, 2025
-
Mary Is A Department Of The Navy Employee
Mar 30, 2025
-
James Bond In A Honda Answer Key
Mar 30, 2025
-
Ready Player One How Many Chapters
Mar 30, 2025
-
Identifying Transformations Worksheet Homework 5 Answer Key
Mar 30, 2025
Related Post
Thank you for visiting our website which covers about An Index Of Suspicion Is Most Accurately Defined As . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
