Anaphylaxis Is Most Accurately Defined As An
Onlines
Mar 25, 2025 · 7 min read
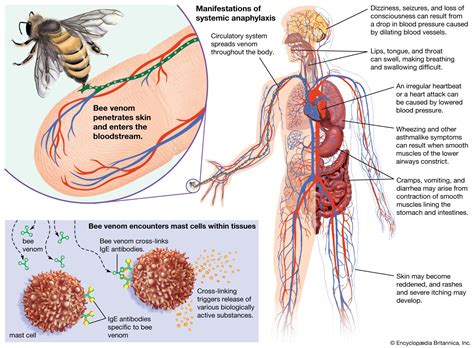
Table of Contents
Anaphylaxis: A Comprehensive Overview of the Most Accurate Definition and Management
Anaphylaxis is a severe, life-threatening allergic reaction that can occur within seconds or minutes of exposure to an allergen. Understanding its accurate definition, triggers, symptoms, diagnosis, and treatment is crucial for both healthcare professionals and individuals at risk. This article will delve into the complexities of anaphylaxis, providing a comprehensive overview for a thorough understanding.
Defining Anaphylaxis: More Than Just a Severe Allergic Reaction
While often described as a severe allergic reaction, anaphylaxis is more accurately defined as a systemic, life-threatening hypersensitivity reaction characterized by a rapid onset and potentially fatal outcome. This crucial distinction highlights the urgency and gravity of the condition. It isn't simply an escalation of mild allergy symptoms; it's a distinct clinical entity demanding immediate intervention.
The precise definition has evolved, reflecting advancements in understanding its pathophysiology. Key characteristics underpinning the most accurate definition include:
- Rapid onset: Symptoms usually appear within minutes of exposure, although a delayed reaction is possible, sometimes up to several hours.
- Systemic involvement: Multiple organ systems are affected, including the skin, respiratory system, cardiovascular system, and gastrointestinal tract. This systemic nature differentiates it from localized allergic reactions.
- Life-threatening potential: Anaphylaxis can lead to airway compromise, cardiovascular collapse, and death if not treated promptly.
- Hypersensitivity reaction: It's an exaggerated immune response triggered by the interaction of an allergen with pre-sensitized IgE antibodies on mast cells and basophils, leading to the release of inflammatory mediators.
Several professional organizations, like the World Allergy Organization (WAO) and the American Academy of Allergy, Asthma & Immunology (AAAAI), have contributed to refining the definition, emphasizing the need for a multi-system approach in diagnosis and management. The current consensus emphasizes the rapid onset of symptoms affecting at least two organ systems and the potential for life-threatening outcomes.
Common Triggers of Anaphylaxis: Identifying Potential Hazards
Understanding the common triggers is crucial in prevention and management. These triggers vary widely among individuals, with some exhibiting sensitivities to multiple allergens. The most prevalent triggers include:
Foods:
- Nuts (peanuts, tree nuts): A leading cause of anaphylaxis, particularly in children. Even trace amounts can trigger a reaction in highly sensitive individuals.
- Shellfish (crustaceans, mollusks): Another significant food allergen, often causing severe reactions.
- Milk: A common allergen in young children, but reactions can persist into adulthood.
- Eggs: Frequently encountered in baked goods and other foods, posing a risk for allergic individuals.
- Soy: Found in many processed foods, soy products can trigger anaphylaxis.
- Wheat: While less likely to cause severe reactions than other food allergens, wheat can still trigger anaphylaxis in some individuals.
- Fish: Similar to shellfish, fish can also cause severe allergic reactions in sensitive individuals.
Medications:
- Penicillin and other beta-lactam antibiotics: These are among the most common medication triggers for anaphylaxis.
- Nonsteroidal anti-inflammatory drugs (NSAIDs): Such as ibuprofen and aspirin, can induce anaphylactic reactions in susceptible individuals.
- Contrast dyes: Used in medical imaging, these dyes can trigger reactions, sometimes severe.
- Chemotherapy drugs: Certain chemotherapy agents can induce anaphylaxis.
Insect stings and bites:
- Hymenoptera stings (bees, wasps, hornets, ants): These are frequent causes of anaphylaxis, especially in individuals with pre-existing sensitization.
Other Triggers:
- Latex: Exposure to latex products, such as gloves or balloons, can trigger severe reactions.
- Exercise-induced anaphylaxis: This type of anaphylaxis is triggered by a combination of allergen exposure and physical exertion.
- Idiopathic anaphylaxis: In some cases, the trigger for anaphylaxis cannot be identified, making prevention challenging.
Recognizing the Symptoms of Anaphylaxis: A Crucial First Step
The diverse range of symptoms makes early recognition vital. The speed of onset and the severity of symptoms vary significantly between individuals and exposures. Recognizing even a subset of symptoms should prompt immediate medical intervention.
Common Symptoms:
- Skin and mucosal manifestations: Hives (urticaria), itching, flushing, swelling (angioedema), particularly around the lips, tongue, and throat.
- Respiratory symptoms: Wheezing, shortness of breath, coughing, difficulty swallowing or speaking, feeling of a tight throat.
- Cardiovascular symptoms: Rapid pulse, dizziness, lightheadedness, fainting, hypotension (low blood pressure), cardiac arrest.
- Gastrointestinal symptoms: Nausea, vomiting, abdominal cramps, diarrhea.
Less Common Symptoms:
- Neurological symptoms: Loss of consciousness, confusion, headache.
- Urinary symptoms: Urinary incontinence.
It's crucial to note that not all individuals will experience all symptoms. Some may only exhibit mild symptoms like hives, while others might experience a rapid and catastrophic cascade of symptoms leading to cardiovascular collapse. Any combination of symptoms, especially if they develop rapidly after exposure to a potential allergen, warrants immediate medical attention.
Diagnosing Anaphylaxis: A Multifaceted Approach
Diagnosing anaphylaxis relies on a combination of clinical presentation, patient history, and potentially supportive laboratory investigations.
- Clinical history: A detailed history focusing on the temporal relationship between exposure to a potential allergen and the onset of symptoms is paramount. The speed of symptom onset, the severity of symptoms, and the involvement of multiple organ systems are all key diagnostic features.
- Physical examination: A thorough physical examination should assess the patient's vital signs (blood pressure, heart rate, respiratory rate), skin and mucosal lesions, and level of consciousness.
- Laboratory investigations: While not always necessary for diagnosis, laboratory tests may provide supporting evidence. These can include measuring serum tryptase levels (although elevated levels are not always specific to anaphylaxis), performing blood counts, and checking for the presence of specific IgE antibodies to suspected allergens.
A thorough clinical assessment is the cornerstone of diagnosing anaphylaxis. While laboratory tests may provide supportive information, the diagnosis is primarily based on clinical presentation.
Managing Anaphylaxis: A Priority for Immediate Action
Treatment of anaphylaxis is a critical medical emergency. The primary goal is to stabilize the patient’s airway, breathing, and circulation. Delay in treatment can be fatal.
Immediate Actions:
- Administer epinephrine (adrenaline): This is the cornerstone of anaphylaxis treatment. Epinephrine should be administered intramuscularly (into the thigh) as quickly as possible. Auto-injectors, such as EpiPens, are commonly used for self-administration or administration by bystanders.
- Maintain airway patency: If airway compromise occurs, measures such as supplemental oxygen, intubation, and mechanical ventilation may be necessary.
- Support circulation: Intravenous fluids may be administered to improve blood pressure and maintain circulation.
- Monitoring: Continuous monitoring of vital signs, including blood pressure, heart rate, respiratory rate, and oxygen saturation is crucial.
- Further medical care: Emergency medical services (EMS) should be contacted immediately. Hospitalization is often necessary for close observation and further management.
Subsequent Management:
- Further doses of epinephrine: If symptoms don't improve or recur, further doses of epinephrine may be required.
- Antihistamines: These medications can help manage skin and mucosal symptoms, but they are not a substitute for epinephrine.
- Corticosteroids: These medications reduce inflammation and can help prevent late-phase reactions.
- Further investigations: Once stabilized, additional tests may be conducted to identify the allergen and develop a long-term management plan.
Preventing Anaphylaxis: Proactive Strategies
Prevention is paramount in managing anaphylaxis. Strategies focus on identifying triggers, avoiding exposure, and having a readily available emergency plan.
- Allergen identification and avoidance: Detailed allergy testing can identify specific triggers. Careful avoidance of identified allergens is essential.
- Emergency preparedness: Individuals at risk should always carry epinephrine auto-injectors, along with instructions on their use. A written anaphylaxis action plan, outlining steps to take in case of a reaction, should be developed in consultation with an allergist.
- Education and training: Patients, family members, and bystanders should receive education about recognizing the symptoms of anaphylaxis and the proper use of epinephrine.
- Medical alert bracelets or necklaces: These serve as a visible reminder to healthcare professionals in the event of a reaction.
Conclusion: A Call for Understanding and Action
Anaphylaxis is a serious, potentially fatal condition. Its accurate definition emphasizes its systemic nature and life-threatening potential. Early recognition of symptoms, prompt administration of epinephrine, and subsequent medical management are critical for saving lives. Prevention through allergen identification, avoidance, and emergency preparedness is a vital aspect of managing this challenging condition. A multidisciplinary approach involving allergists, other healthcare professionals, and individuals at risk is essential in mitigating the risks and improving outcomes. The focus should always remain on early recognition, immediate action, and meticulous follow-up care to ensure patient safety and well-being.
Latest Posts
Latest Posts
-
Anticipating Potential Provider Prescriptions System Disorder
Mar 26, 2025
-
Quotes From The Letter From Birmingham Jail
Mar 26, 2025
-
Chemistry Moles Packet Answer Key Pdf
Mar 26, 2025
-
Nih Stroke Scale Answers Group D
Mar 26, 2025
-
Focused Reports Help Managers Before Recommending Solutions
Mar 26, 2025
Related Post
Thank you for visiting our website which covers about Anaphylaxis Is Most Accurately Defined As An . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
