Industry-wide Standards For Health Claims Bring Simplification Because
Onlines
Mar 27, 2025 · 6 min read
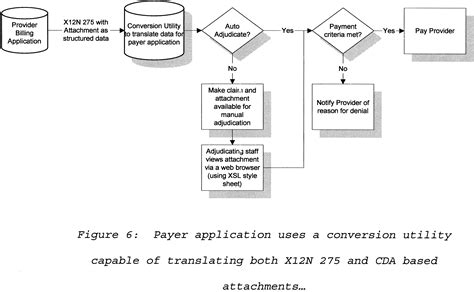
Table of Contents
Industry-Wide Standards for Health Claims Bring Simplification Because…
The healthcare industry is notorious for its complexity. Navigating insurance plans, understanding billing codes, and submitting accurate health claims can feel like traversing a labyrinthine maze. This complexity impacts everyone – patients, providers, and payers alike. However, the rising adoption of industry-wide standards for health claims is beginning to illuminate this maze, offering a pathway toward unprecedented simplification. This simplification isn't merely a convenience; it's a crucial step toward improving efficiency, reducing costs, and ultimately, improving patient care.
The Current State of Chaos: Why Simplification is Crucial
Before delving into the benefits of standardization, it's essential to understand the current landscape. The lack of uniform standards has historically led to a fragmented system characterized by:
1. Inconsistent Data Formats and Coding:
Different payers (insurance companies) often use varying data formats and coding systems for health claims. This means providers must adapt their systems and processes to each payer, increasing administrative burden and the potential for errors. A single claim might require multiple versions, depending on the destination.
2. High Administrative Costs:
The manual effort required to adapt to different payer requirements significantly increases administrative costs for providers. This cost is ultimately passed on to patients in the form of higher healthcare expenses. Staff time is consumed managing discrepancies, resolving rejections, and chasing payments.
3. Increased Risk of Errors and Denials:
The complexity of the system leads to a higher probability of errors in claim submissions. Even minor inaccuracies can result in claim rejections, delays in payment, and disputes with payers. This adds to the frustration for both providers and patients.
4. Lack of Interoperability:
The absence of unified standards hinders the seamless exchange of healthcare information between different systems and stakeholders. This limitation hampers the ability to provide coordinated and comprehensive care. Imagine a scenario where a specialist can't readily access a patient's complete medical history due to incompatible systems.
5. Inefficient Resource Allocation:
Resources are wasted on resolving issues stemming from inconsistent claim processing. This includes time spent on manual data entry, reconciliation, and follow-up with payers. These inefficiencies drain resources that could be better allocated to direct patient care.
The Promise of Standardization: Streamlining the Health Claims Process
Industry-wide standards offer a solution to this chaos. By adopting common formats and protocols, the healthcare industry can dramatically simplify the process of submitting, processing, and paying health claims. This leads to several key benefits:
1. Reduced Administrative Burden:
Standardized claim formats eliminate the need for providers to customize claims for each payer. This significantly reduces the administrative burden, freeing up staff to focus on patient care instead of paperwork. Think of it as the difference between writing a different letter for each recipient versus using a templated email with personalized details.
2. Lower Administrative Costs:
With streamlined processes and reduced errors, administrative costs are drastically lowered. This translates to lower healthcare expenses for everyone. The savings can be reinvested into improving patient care or lowering overall healthcare costs.
3. Improved Accuracy and Reduced Denials:
Standardization minimizes the risk of errors in claim submissions, leading to fewer rejections and faster payment processing. This improves cash flow for providers and reduces delays in patient care. Automated validation checks within standardized systems can catch errors before submission.
4. Enhanced Interoperability:
Standardized data formats enable seamless information exchange between different systems. This improves coordination of care, facilitates data analysis, and allows for better decision-making based on comprehensive patient data. Imagine seamless data sharing between a primary care physician, a specialist, and a hospital system.
5. Improved Data Analytics and Reporting:
Standardized data allows for more effective data analysis and reporting. This enables better understanding of healthcare trends, identification of areas for improvement, and more informed decision-making by healthcare providers and payers. This data-driven approach leads to more efficient resource allocation.
Key Standards Driving Simplification
Several key standards are driving the simplification of health claims processes:
1. HIPAA (Health Insurance Portability and Accountability Act):
While not exclusively focused on claim standardization, HIPAA plays a critical role by establishing national standards for electronic healthcare transactions, including claims. It sets the groundwork for interoperability and data security.
2. HL7 (Health Level Seven):
HL7 is a widely adopted standard that defines messaging formats for exchanging healthcare information electronically. Its various versions, such as FHIR (Fast Healthcare Interoperability Resources), are designed to facilitate interoperability and streamline communication between different systems. FHIR is particularly important for its focus on API-driven communication.
3. X12:
X12 is another standard used for electronic data interchange (EDI) in healthcare. It defines the structure and content of various healthcare transactions, including claims. While older than HL7, it's still widely used and integral to many existing systems.
4. ICD (International Classification of Diseases):
ICD codes are used to classify diseases and medical conditions. Their consistent use across different systems is vital for accurate claim processing and data analysis. The latest version, ICD-11, is designed to improve precision and interoperability.
5. CPT (Current Procedural Terminology):
CPT codes are used to report medical procedures and services. Their standardization is essential for accurate billing and claim processing. Consistent CPT coding is vital for minimizing errors and discrepancies.
Overcoming Barriers to Full Standardization
Despite the significant benefits, achieving full standardization across the healthcare industry faces several challenges:
1. Legacy Systems:
Many healthcare providers and payers rely on older systems that are not compatible with modern standards. Upgrading these systems can be expensive and time-consuming.
2. Resistance to Change:
There can be resistance to adopting new standards from organizations accustomed to their existing processes. Overcoming inertia requires education, incentives, and strong leadership.
3. Interoperability Issues:
Even with standardized formats, achieving seamless interoperability between different systems can be technically challenging. This requires careful planning, testing, and ongoing maintenance.
4. Data Security and Privacy Concerns:
The increased exchange of electronic health information necessitates robust security measures to protect patient data privacy and confidentiality. Compliance with regulations like HIPAA is crucial.
5. Cost of Implementation:
Implementing new systems and adopting new standards can be costly. This can be a barrier for smaller healthcare providers, particularly in resource-constrained settings.
The Future of Health Claim Standardization: A Simplified Landscape
The future of health claims processing is undeniably moving towards greater standardization. The long-term benefits far outweigh the challenges. Continued efforts to improve interoperability, promote the adoption of modern standards, and address the technical and financial barriers will lead to a more simplified, efficient, and cost-effective healthcare system. This ultimately leads to better patient care and a more sustainable healthcare ecosystem.
The move toward standardization isn't just about simplifying claims processing; it's about transforming the healthcare industry into a more data-driven, patient-centric, and interconnected system. This improved ecosystem empowers better care, optimized resource allocation, and ultimately, healthier populations. The path may be challenging, but the destination — a simplified and efficient healthcare landscape—is worth pursuing. The ongoing development and implementation of industry-wide standards are paving the way for a healthier and more efficient future for all.
Latest Posts
Latest Posts
-
Pal Histology Muscular Tissue Lab Practical Question 9
Mar 30, 2025
-
La Natacion Bucear Esquiar El Parque
Mar 30, 2025
-
Peptic Ulcer Disease Hesi Case Study
Mar 30, 2025
-
A Covered Entity Must Have An Established Complaint Process
Mar 30, 2025
-
Knowledge Drill 11 4 Glucose Tolerance Test
Mar 30, 2025
Related Post
Thank you for visiting our website which covers about Industry-wide Standards For Health Claims Bring Simplification Because . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
