Nursing Care Plan For Neonatal Hyperbilirubinemia
Onlines
Mar 25, 2025 · 6 min read
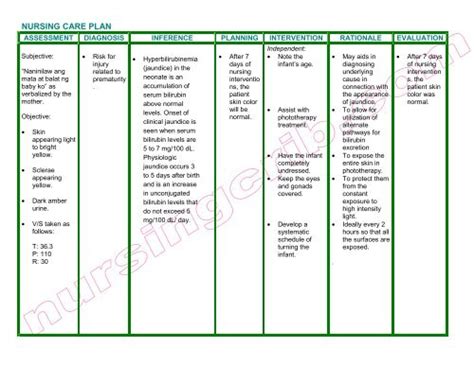
Table of Contents
Nursing Care Plan for Neonatal Hyperbilirubinemia
Neonatal hyperbilirubinemia, or jaundice, is a common condition affecting newborns, characterized by a yellowish discoloration of the skin and whites of the eyes due to elevated bilirubin levels. While often benign and resolving spontaneously, hyperbilirubinemia can lead to serious complications if left untreated, particularly kernicterus, a form of bilirubin encephalopathy. Therefore, a comprehensive nursing care plan is crucial for effective management and prevention of adverse outcomes. This plan focuses on early detection, appropriate interventions, and family education to ensure optimal neonatal health.
Assessment: The Foundation of Care
A thorough assessment forms the bedrock of any effective nursing care plan. For neonatal hyperbilirubinemia, this involves:
1. History Taking:
- Maternal History: Detailed maternal history, including prenatal care, gestational age, mode of delivery, maternal blood type, and any history of hyperbilirubinemia in previous pregnancies. This is crucial as certain factors like ABO incompatibility, Rh incompatibility, and prematurity can significantly increase the risk of hyperbilirubinemia.
- Neonatal History: Assessment of the newborn's gestational age, birth weight, feeding patterns, bowel movements (meconium passage), and any signs of distress. Premature infants are at higher risk due to immature liver function. Delayed meconium passage can also contribute to hyperbilirubinemia.
- Family History: A family history of jaundice can indicate a genetic predisposition.
2. Physical Examination:
- Visual Assessment: Careful observation for the presence and extent of jaundice, starting from the face and progressing downwards. The intensity and distribution of jaundice can provide clues about the severity of hyperbilirubinemia. Assess for other signs like lethargy, poor feeding, and irritability.
- Vital Signs: Monitoring heart rate, respiratory rate, temperature, and blood pressure. Dehydration can exacerbate hyperbilirubinemia, hence, careful monitoring is essential.
- Neurological Assessment: Observing for signs of central nervous system involvement, such as hypotonia, lethargy, poor suck, high-pitched cry, and opisthotonos. These could indicate kernicterus, a serious complication.
Diagnosing Hyperbilirubinemia: Beyond Visual Inspection
Visual assessment alone is insufficient for diagnosing and managing hyperbilirubinemia. Laboratory investigations are crucial:
- Total Serum Bilirubin: This is the primary diagnostic test measuring the total amount of bilirubin (both direct and indirect) in the blood.
- Direct and Indirect Bilirubin: Differentiating between direct (conjugated) and indirect (unconjugated) bilirubin helps determine the type and potential cause of hyperbilirubinemia. Unconjugated hyperbilirubinemia is the most common form in newborns.
- Blood Type and Rh Factor: Determining the mother's and infant's blood types and Rh factors is essential to rule out blood group incompatibility, a significant cause of hyperbilirubinemia.
- Coombs' Test: This test detects the presence of antibodies in the infant's blood, often indicating Rh incompatibility.
- Other Tests: Depending on clinical suspicion, additional tests might include complete blood count (CBC), liver function tests (LFTs), and blood cultures to rule out underlying infections.
Nursing Interventions: A Multifaceted Approach
The nursing care plan for neonatal hyperbilirubinemia is multifaceted, focusing on preventative measures, treatment interventions, and continuous monitoring.
1. Phototherapy:
Phototherapy is a common treatment for hyperbilirubinemia. It uses special lights to convert unconjugated bilirubin into a water-soluble form that can be excreted in the urine and feces. Nursing responsibilities include:
- Positioning: Frequent repositioning of the infant is crucial to ensure even exposure to the light, minimizing skin breakdown. Eye protection is essential to prevent retinal damage.
- Monitoring: Closely monitor the infant's temperature, hydration status, and skin condition. Phototherapy can cause dehydration and skin breakdown.
- Fiber Optic Pads: In cases where traditional phototherapy is not sufficient, fiber optic pads might be used for more targeted illumination.
- Documentation: Meticulous documentation of phototherapy duration, intensity, and the infant's response is essential.
2. Exchange Transfusion:
Exchange transfusion is a more invasive procedure used in severe cases of hyperbilirubinemia, especially when there's a risk of kernicterus. It involves replacing the infant's blood with donor blood to rapidly lower bilirubin levels. Nursing responsibilities include:
- Pre-procedure care: Ensuring the infant is adequately prepared and monitored.
- Post-procedure care: Closely monitoring vital signs, observing for complications such as bleeding or infection, and providing supportive care.
3. Hydration and Feeding:
Adequate hydration and feeding are crucial to promote bilirubin excretion.
- Breastfeeding: Encouraging frequent breastfeeding helps stimulate bowel movements and bilirubin excretion.
- Formula Feeding: For infants not breastfeeding, ensuring appropriate formula intake is essential.
- Hydration: Maintaining adequate hydration by monitoring intake and output. Fluid restriction is generally not recommended.
4. Monitoring for Complications:
Continuous monitoring for potential complications is paramount.
- Kernicterus: Regular neurological assessments are crucial to detect early signs of kernicterus.
- Dehydration: Closely monitoring hydration status through weight monitoring, urine output, and assessing skin turgor.
- Hypothermia: Phototherapy can cause heat loss; hence, maintaining optimal temperature is essential.
- Skin Breakdown: Frequent skin assessments and appropriate skin care are necessary to prevent skin breakdown.
Family Education: Empowerment and Support
Educating the family is a vital aspect of the nursing care plan. This empowers parents to actively participate in their infant's care and understand the condition's progression and management.
- Understanding Hyperbilirubinemia: Providing clear and concise information about the cause, progression, and treatment of neonatal hyperbilirubinemia.
- Phototherapy Explanation: Explaining the purpose, procedure, and potential side effects of phototherapy.
- Feeding Guidance: Providing guidance on appropriate feeding techniques, whether breastfeeding or formula feeding.
- Monitoring for Complications: Educating parents on signs and symptoms to watch for, emphasizing the importance of immediate medical attention if any concerns arise.
- Follow-up Care: Informing parents about the need for follow-up appointments to monitor bilirubin levels and ensure the condition resolves completely.
- Emotional Support: Providing emotional support to alleviate parental anxieties and concerns about their baby's condition.
Documentation and Collaboration: A Team Effort
Accurate and timely documentation is crucial for seamless care coordination. This includes recording:
- Assessment findings: Detailed documentation of physical assessment findings, including jaundice severity, vital signs, and neurological status.
- Laboratory results: Recording of all laboratory results, including total and indirect bilirubin levels.
- Interventions: Documentation of all interventions, including phototherapy duration, feeding patterns, and any medications administered.
- Response to treatment: Regular recording of the infant's response to treatment, including changes in bilirubin levels and clinical status.
Effective collaboration with other healthcare professionals, including neonatologists, pediatricians, and other nurses, is essential for optimal management of neonatal hyperbilirubinemia. Regular communication and shared decision-making ensures the best possible outcomes for the infant.
Preventing Hyperbilirubinemia: Proactive Measures
While not all cases of hyperbilirubinemia are preventable, certain proactive measures can reduce the risk:
- Early Initiation of Breastfeeding: Encouraging early and frequent breastfeeding stimulates bowel movements, which promotes bilirubin excretion.
- Proper Hydration: Ensuring adequate hydration through breastfeeding or formula feeding helps facilitate bilirubin excretion.
- Identifying Risk Factors: Screening for risk factors, such as prematurity and blood group incompatibility, allows for early intervention.
- Early Detection: Performing regular bilirubin screenings, especially in high-risk infants, can enable prompt treatment.
Conclusion:
Neonatal hyperbilirubinemia requires a comprehensive nursing care plan that encompasses meticulous assessment, appropriate interventions, diligent monitoring, and effective family education. By focusing on early detection, prompt treatment, and proactive preventive measures, nurses play a pivotal role in minimizing the risks associated with this common neonatal condition and ensuring the well-being of the newborn. A collaborative, multidisciplinary approach, combined with thorough documentation, is critical for achieving optimal patient outcomes. Remember, the goal is not just to treat the hyperbilirubinemia but to support the family and ensure the healthy development of the newborn.
Latest Posts
Latest Posts
-
Consider The Following Incomplete Deposit Ticket
Mar 27, 2025
-
What Best Characterizes The Shivercrat Movement
Mar 27, 2025
-
What Transaction Code Is Used To Modify The Users Profile
Mar 27, 2025
-
Math 1325 010 San Antonio Community College
Mar 27, 2025
-
Identify The Syllable Types In The Word Garden
Mar 27, 2025
Related Post
Thank you for visiting our website which covers about Nursing Care Plan For Neonatal Hyperbilirubinemia . We hope the information provided has been useful to you. Feel free to contact us if you have any questions or need further assistance. See you next time and don't miss to bookmark.
